J Cell Physiol:达格列净通过调节AMPK/mTOR信号通路改善肥胖大鼠胰腺损伤并激活肾脏自噬
2021-11-05 从医路漫漫 MedSci原创
由于高血糖、胰岛素抵抗和糖尿病(T2DM)等并发症的存在,肥胖已成为全球主要的健康负担。
由于高血糖、胰岛素抵抗和糖尿病(T2DM)等并发症的存在,肥胖已成为全球主要的健康负担。一些研究表明,长期食用高脂饮食(HF)不仅会导致肥胖和胰岛素抵抗,而且还会导致胰腺的组织病理学改变。在T2DM的早期阶段,胰腺β细胞通过增加β细胞数量来适应胰岛素的需求,这与T2 DM的早期阶段非常相似。在T2DM的最初阶段,胰腺β细胞通过增加β细胞数量来适应胰岛素控制的增加,导致肥胖和胰岛素抵抗期间胰岛素分泌增加。然而,胰岛素的需求持续增加可通过脂质和葡萄糖毒性、氧化应激和慢性炎症导致胰腺β细胞凋亡,导致高血糖时β细胞减少。本文主要研究了钠-葡萄糖共转运体2 (SGLT2)抑制剂达格列净对肥胖患者肾脏和胰腺损伤的影响。
用高脂饲料喂养大鼠16周。分别以1.0 mg/(kg·d)或3.0 mg/(kg·d)达格列净或维格列汀灌胃,疗程4周。探讨达格列净对高脂饮食诱导的肥胖大鼠胰岛素抵抗、肾脏自噬、胰腺氧化应激、内质网应激、炎症反应和细胞凋亡的影响。
磁共振成像(MRI)采集:第16周结束时,大鼠经腹腔注射40 mg/kg戊巴比妥(单剂量)麻醉,俯卧位置于1.5特斯拉磁共振成像扫描仪(Ingenia, Philips Medical Systems)。通过MRI线圈获得腹部区域T1加权冠状或横向图像。腹部图像采集步骤如下。1. 受试者在MR躺椅上以头朝上的姿势俯卧。2. MRI线圈覆盖整个腹部,定位激光位于腹部中部。3.通过T1加权Turbo Fast Echo (TFE)序列获取3毫米厚的腹部图像。
胰腺组织脂质过氧化的测定:简单地说,胰腺组织被切片并浸泡在CelLytic™MT细胞裂解试剂(Sigma‐Aldrich)中,该试剂包含1%完全蛋白酶抑制剂鸡尾酒(罗氏应用科学)。组织均质,4℃,1600g离心10 min。收集上清液,使用硫代巴比妥酸反应物质测定试剂盒测定胰腺组织中丙二醛(MDA)浓度。蛋白浓度使用Bradford蛋白测定试剂盒(Bio‐Rad Laboratories)测定。MDA含量以nmol/mg蛋白表达。
免疫印迹分析:制备胰腺或肾组织的裂解液匀浆。用十二烷基硫酸钠聚丙烯酰胺凝胶电泳(10-15%凝胶)分离每个样品中的蛋白质,用转移缓冲液转移到聚偏氟乙烯膜(Millipore)上。用脱脂牛奶溶液在室温下封膜1小时,用特异性一抗在4°C下探针过夜。用含0.1% Tween 20 (TBS‐T)溶液的三‐缓冲盐水清洗膜三次,并与辣根过氧化物酶偶联的山羊抗兔或抗小鼠二抗(Millipore)在室温下孵育1小时,并使用增强化学发光剂(Bio‐Rad实验室)开发膜。通过暴露于Hyperfilm (GE Healthcare Limited)或iBright™FL1000成像系统(Thermo Fisher Scientific)检测化学发光信号。最后,使用Image J程序确定β‐肌动蛋白密度。
高脂饮食喂养的大鼠出现代谢异常,包括体重、内脏脂肪体重、血浆胰岛素、血浆胆固醇、稳态模型评估(HOMA)指数和TAUCg增加,表明存在肥胖胰岛素抵抗和葡萄糖不耐受情况。此外,高脂饮食喂养的大鼠表现出明显的胰腺损伤,并伴有肾脏自噬减少。达格列净或维格列汀治疗4周可改善肥胖大鼠胰腺氧化应激、内质网应激、炎症和细胞凋亡,并恢复肾脏自噬。治疗组胰腺和肾脏的形态学改变均有改善。有趣的是,在我们的模型中,达格列净在改善体重、内脏脂肪重量、血浆胆固醇水平和胰腺氧化应激方面的疗效优于维格列汀。
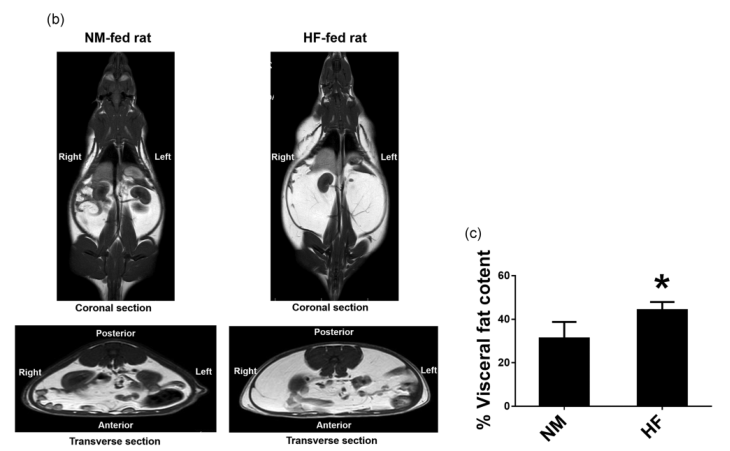
图1 研究方案(a).实验16周内内脏脂肪堆积(白色区域)的体内MRI图像(b, c)。数据以均数±SD表示;n= 6只大鼠/组。* p <。05年和海里。HF、高脂饮食大鼠接受载体治疗;HFDAP,用达格列净处理的高脂饮食大鼠;维格列汀处理的HFVIL高脂饮食大鼠;MRI:磁共振成像;NM,正常饮食大鼠
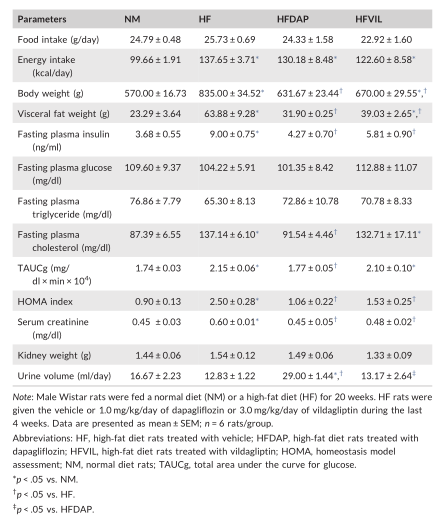
表 达格列净和维格列汀治疗对高脂饮食诱导的肥胖大鼠代谢参数的影响
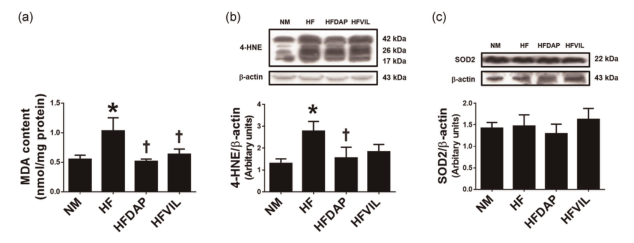
图2 达格列净和维达格列汀治疗对肥胖大鼠胰腺MDA含量(A)、4-HNE(B)和SOD2表达(C)的影响。数据以均值±扫描电镜表示,n=6只/组。*p<0.05对NM;†p<0.05对HF。4-HNE,4-羟基壬烯醛;HF,高脂饮食大鼠;HFDAP,高脂饮食大鼠,达格列净治疗;HFVIL,高脂饮食大鼠,维达格列汀治疗;MDA,丙二醛;NM,正常饮食大鼠;SOD2,超氧化物歧化酶2

图3 达格列净和维达格列汀治疗对肥胖大鼠肾脏p62(A)、LC3B(B)、Beclin-1(C)、Atg5(D)、肾脏H&E染色(E)、肾脏半定量损伤评分(F)、PAS染色(G)和肾小球硬化指数(H)的影响。间质浸润:黑色箭头;水肿间质:绿色箭头;管状间质:红色箭头;核固缩:黄色箭头),数据以平均值±扫描电镜表示;n=6只/组。*p<0.05对NM;†p<0.05对HF。H&E,苏木素染色;HF,高脂饮食大鼠;HFDAP,高脂饮食大鼠,达格列净治疗;HFVIL,高脂饮食大鼠,维达格列汀治疗;NM,正常饮食大鼠;
结论:综上所述,本研究证实达格列净可减轻肥胖大鼠胰腺损伤、胰腺氧化应激、内质网应激、炎症、凋亡,并通过恢复自噬信号通路发挥肾保护作用。
原文出处:
Jaikumkao K, Promsan S, Thongnak L,et al.Dapagliflozin ameliorates pancreatic injury and activates kidney autophagy by modulating the AMPK/mTOR signaling pathway in obese rats.J Cell Physiol 2021 Sep;236(9)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
57
#CEL#
36
#Physio#
54
#损伤#
37
#信号通路#
33