一般来说当在X线片上能够发现骨关节炎的各种表现时,患者通常已经有较长的病程,病情较为严重了。许多朋友会问,那有什么办法能够早期发现关节软骨有无磨损呢?
临床上目前主要有两种办法,一种没有创伤的检查:磁共振;另一种是有创的检查:关节镜。对于怀疑是骨关节炎的患者,大多数首先采取的是磁共振检查,在这个章节中给大家介绍下骨关节炎在磁共振上的各种常见表现。
下面这张膝关节X线片是一位长跑爱好者的,这位患者已经坚持长跑十多年了,从今年开始跑步后膝关节出现疼痛、肿胀,在膝关节屈曲活动时疼痛尤为剧烈。

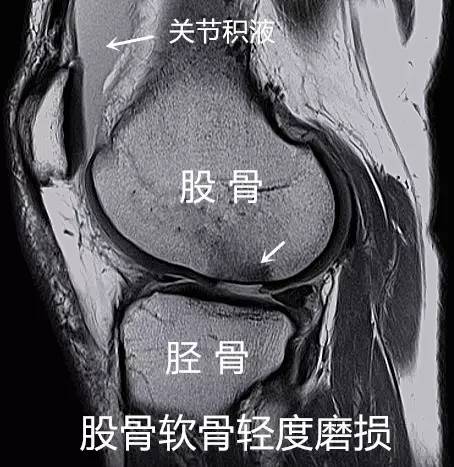
在X线片上,并没有发现什么问题,但继续对患者进行磁共振检查,下图是该患者的膝关节磁共振侧位片,可以看到膝关节腔内存在大量积液,同时最关键的是该患者对应胫骨平台的的股骨髁关节面出现了软骨磨损。软骨磨损程度目前还较轻,不至于影响行走活动,但当该患者进行跑步等剧烈活动后,软骨磨损区域由于受到持续的磨损刺激产生多种致炎因子,导致膝关节出现疼痛及积液。而这种程度的软骨磨损在X线下是完全无法观察到的,如果放任该患者继续锻炼,会导致膝软骨磨损进一步加重,正如后面一系列的磁共振片子所展示的。

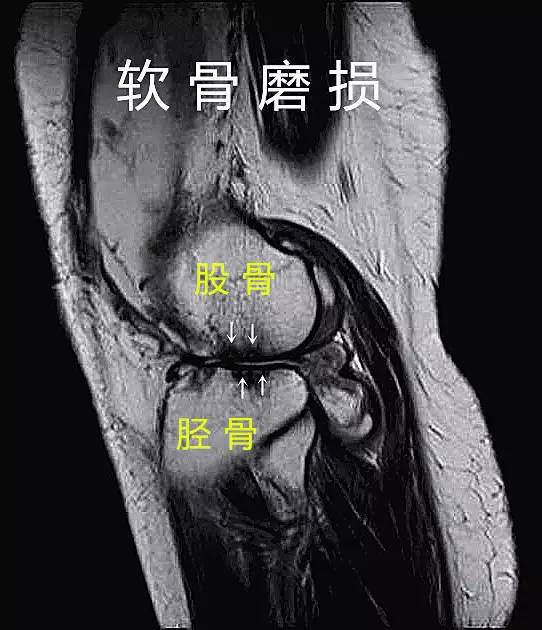
从上面两张磁共振片子中,我们可以看到软骨磨损程度逐渐加重,当软骨磨损较为严重时,可以观测到股骨和胫骨之间的关节间隙狭窄乃至消失,同时可以看到在股骨和胫骨接近的关节面上存在一些密度较低的不规则区域(白色箭头所指),这就是关节表面软骨磨损程度加重直至软骨下骨时的表现,到这种磨损程度时X线片上才能观测到异常表现。因此,磁共振能够较早的观测到关节软骨的改变及早期发现关节软骨磨损。
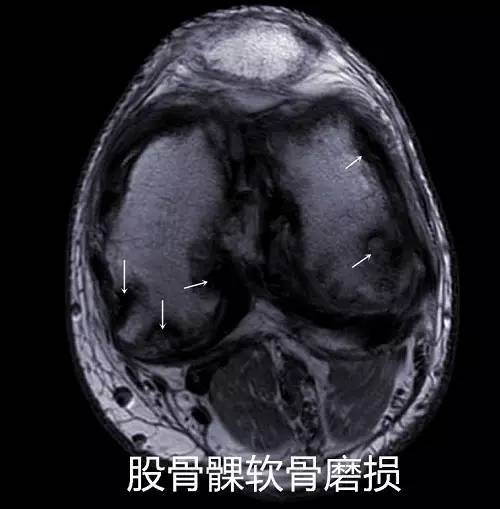
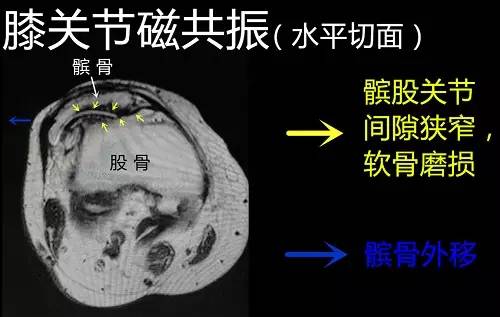
这是一张膝关节磁共振的水平切面,可以看到非常明显的股骨髁软骨磨损,而在X线片上仅仅能够观测到膝关节的前后位和侧位的影像,由于骨组织结构的重叠及遮挡,X线片是无法对关节软骨的磨损程度进行全面评估的。
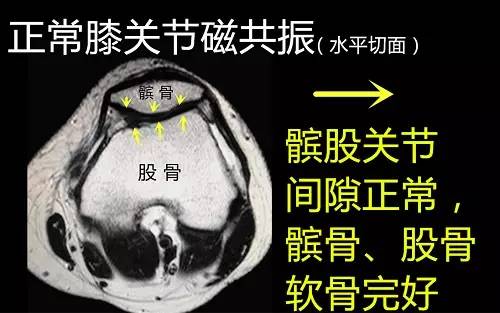
下面是正常膝关节磁共振和骨关节炎磁共振的对比示意图,有助于大家理解骨关节炎的各种异常表现。首先来看看正常膝关节磁共振表现:
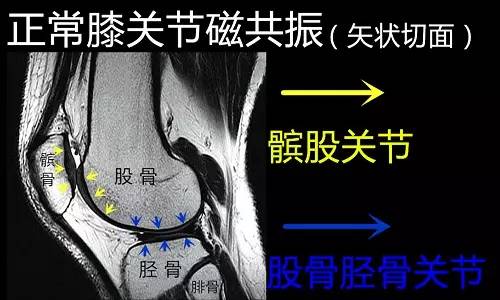
了解了正常的膝关节磁共振表现,接下来就来看看骨关节炎各种常见的磁共振表现。

以上是膝关节骨关节炎在磁共振上的各种常见表现,最后和大家一起看一张严重的骨关节炎患者的磁共振示意图:

在这个章节中介绍了骨关节炎患者的膝关节磁共振表现,除了无创性的磁共振检查,如果碰到膝关节反复肿胀,或是合并半月板、交叉韧带损伤的患者,还可以采取关节镜检查进行诊断和治疗。在下一个章节中,阿土伯将向大家介绍下骨关节炎在关节镜下的各种常见表现。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
43
#关节疼痛#
48
#骨关节#
48
#关节炎#
0
#X线#
0
#X线片#
0