Nat Neurosci:复旦大学张玉秋研究组等揭示PD-1通路抑制疼痛逃避神经系统监视机制
2017-05-25 佚名 生物帮
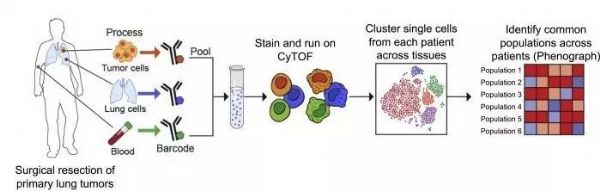
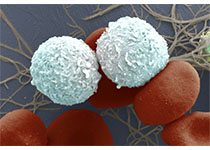
近日,国际学术权威刊物自然出版集团旗下子刊《Nature Neuroscience》杂志在线发表了复旦大学脑科学研究院张玉秋研究组和美国杜克大学季如荣(音译)研究组合作的一篇研究论文,研究论文题为《PD-L1inhibits acute and chronic pain by suppressing nociceptive neuron activity viaPD-1》。研究发现细胞程序性死亡因
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Nat#
26
#神经系统#
43
#ROS#
32
#复旦#
26
还需进一步研究
53
学习了,重视了
54
好好努力学习
53