Diabetologia:同样是胖子为什么有的人就不会患糖尿病?
2016-09-17 佚名 生物谷
每年全世界有大约三百万人的死亡与肥胖及肥胖相关疾病,如糖尿病,癌症和心血管疾病有关。但是有一些肥胖的人似乎可以受到保护不发生这些疾病。深入理解其中的保护性机制有助于为存在疾病高风险的人设计新的治疗策略。在这项发表在国际学术期刊Diabetologia上的研究中,来自英国布里斯托大学等研究机构的研究人员发现健康肥胖个体体内的脂肪干细胞可以更加高效地分化形成脂肪细胞,更加有效地储存脂肪,脂肪的储存效率
每年全世界有大约三百万人的死亡与肥胖及肥胖相关疾病,如糖尿病,癌症和心血管疾病有关。但是有一些肥胖的人似乎可以受到保护不发生这些疾病。深入理解其中的保护性机制有助于为存在疾病高风险的人设计新的治疗策略。
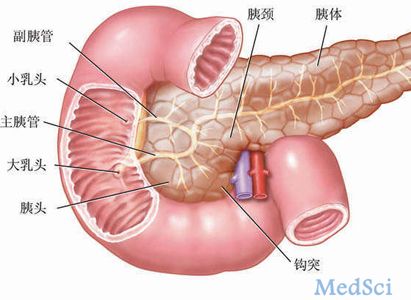
在这项发表在国际学术期刊Diabetologia上的研究中,来自英国布里斯托大学等研究机构的研究人员发现健康肥胖个体体内的脂肪干细胞可以更加高效地分化形成脂肪细胞,更加有效地储存脂肪,脂肪的储存效率高于那些存在糖尿病高风险的肥胖病人。
参与该研究的Dr. Wael Kafienah这样解释道:“糖尿病低风险肥胖个体的存在在过去几年里面得到了许多关注,这些人可能掌握了理解甚至有可能治疗肥胖相关糖尿病的线索。我们的临床数据也确实证实了之前报道的肥胖相关病理学的可变性。在这项新研究中我们证明了体内存在健康脂肪干细胞的肥胖个体有更低的胆固醇水平和更好的肝功能。”
另外一位研究人员Dr .Mohamed Elrayess表示:“在这项研究中我们已经证明血液中炎症性因子IL-6的升高会导致脂肪干细胞分化形成脂肪细胞的能力受到损伤。我们也在体外实验中发现从健康肥胖个体体内分离出来的脂肪干细胞暴露在含有IL-6的实验环境下,这些细胞形成脂肪细胞的能力也会像那些从糖尿病高风险人群体内获得的脂肪干细胞一样受到损伤。”
这项研究着重强调了脂肪干细胞在糖尿病发生过程中的重要性。研究人员表示他们将继续探索提高脂肪干细胞分化效率的新方式,帮助降低处于糖尿病前期的肥胖病人罹患糖尿病的风险。
原始出处
Shamma Almuraikhy, Wael Kafienah, Moataz Bashah, Ilhame Diboun, Morana Jaganjac, Fatima Al-Khelaifi, Houari Abdesselem, Nayef A. Mazloum, Mohammed Alsayrafi, Vidya Mohamed-Ali, Mohamed A. Elrayess.Interleukin-6 induces impairment in human subcutaneous adipogenesis in obesity-associated insulin resistance.Diabetologia.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#DIA#
13
#BET#
15
总结的很好!
40
分享一下!
39
学习了,很受益,谢谢分享,继续关注中!
49
文章很好,非常有益
31
每个人的先后天环境不同。
43
可能基因及后天因素差异所致!
13