Eur Urol:长期筛查项目中,年龄、前列腺癌风险和较高Gleason评分之间的关系
2022-02-19 AlexYang MedSci原创
在Göteborg-1随机、基于人群的PC筛查试验中,调查了年龄、前列腺癌风险和较高Gleason评分之间的关系。
众所周知,年龄是前列腺癌(PC)发病的风险因素。最重要的预后变量-Gleason评分(GS)也与诊断时的年龄有关。早期研究主要是基于流行性筛查男性的数据,而不是基于重复筛查的结果,使得流行性筛查结果与实际发病率的出入风险增加。目前还不清楚年龄和GS之间的相关性是由于生物学上的差异还是诊断过程的选择,例如,老年男性的活检门槛较高,诊断时间较长,肿瘤较晚。

既往的研究表明较大的年龄,前列腺癌(PC)的风险的增加以及较高的Gleason评分之间可能存在关联。最近,来自瑞典的研究人员在《Eur Urol》上发表文章,在Göteborg-1随机、基于人群的PC筛查试验中调查了这些关联。
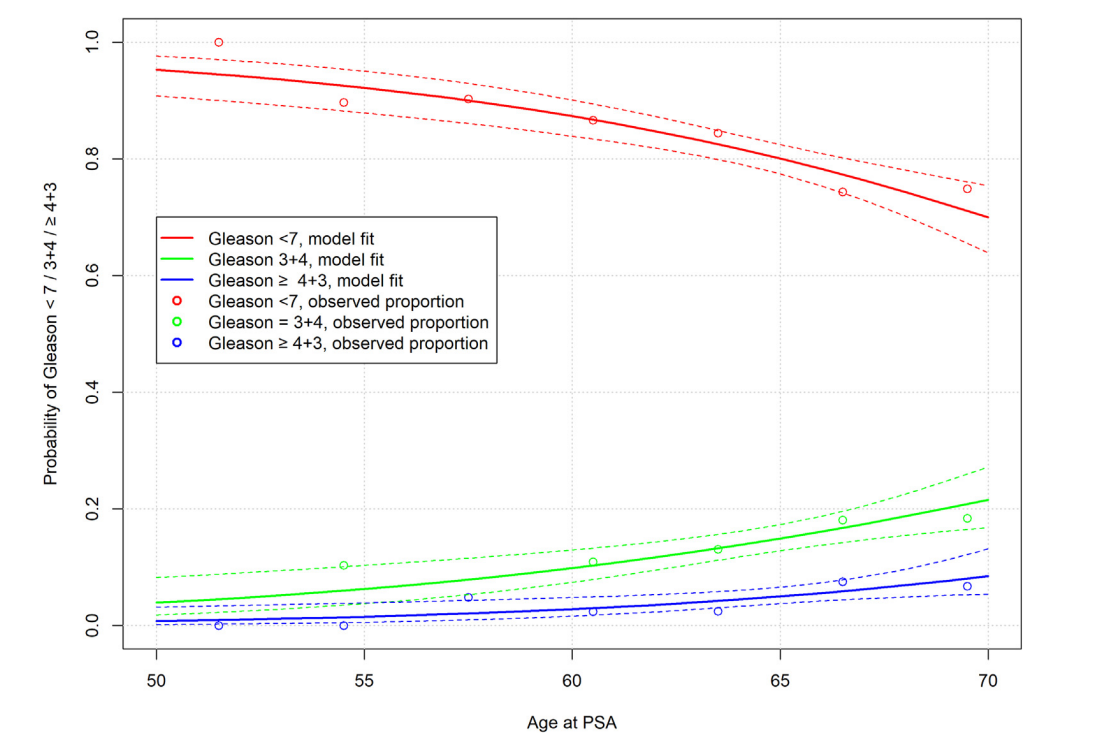
G?teborg-1筛查试验的队列由瑞典哥德堡地区随机选择的10000名男性(年龄50-64岁)组成。1995年至2014年期间,他们每两年进行一次前列腺特异性抗原(PSA)检测,检测的年龄上限为70岁(范围67-71岁)。PSA≥3 ng/ml时会进行前列腺活检(1995-2009年为六处定位活检,此后为十芯活检)。研究人员使用多项逻辑回归分析,调查了年龄对Gleason评分的影响,考虑了筛查出的PC,并对检测年份和筛查回合进行了调整。
总体来说,有7625名男性至少进行了一次PSA检测,1022名男性诊断为PC。对于筛查出PC的男性来说,年龄与临床显著性PC风险的相关性大于筛查的回合和检测的年份(P < 0.001)。年龄每增加1岁,诊断为Gleason评分≥3+4癌症(vs <7)的风险增加11%(95%置信区间[CI]4.7-17);而诊断为Gleason评分≥4+3的癌症(vs <7)的风险则增加8.5%(95%CI-1.6至20)。
诊断为前列腺癌的男性中
综上所述,在男性进行PC早期诊断和治疗的咨询时,应考虑到老年男性较高Gleason评分风险的增加。
原始出处:
Rebecka Arnsrud Godtman, Karin Stinesen Kollberg, Carl-Gustaf Pihl et al. The Association Between Age, Prostate Cancer Risk, and Higher Gleason Score in a Long-term Screening Program: Results from the Göteborg-1 Prostate Cancer Screening Trial. Eur Urol. Feb 2022
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#癌风险#
73
#Gleason评分#
49
#前列腺癌风险#
49
#ASO#
45
#前列腺癌#
130
#筛查项目#
45