国内研究:什么?胃里的细菌与动脉粥样硬化也有关?
2018-05-09 卢芳 中国循环杂志
幽门螺旋杆菌(HP)是伤胃“大户”,事实上其危害不止于胃,还会“伸手”到心血管。
幽门螺旋杆菌(HP)是伤胃“大户”,事实上其危害不止于胃,还会“伸手”到心血管。
重庆学者陈玲等对9项病例对照研究进行的Meta分析则显示,幽门螺旋杆菌阳性者的颈动脉内膜中层厚度高于幽门螺旋杆菌阴性者。
进一步分析发现,幽门螺旋杆菌感染与颈动脉内膜中层厚度有关,可以使颈动脉内膜增厚。
据悉,HP可能通过引起机体持续低度炎性反应及宿主肽蛋白的分子表达模拟机制等来参与胃肠外疾病。而王德昭等进行这项研究中,感染HP的心梗患者高敏C反应蛋白也明显升高。
之前还有多项研究在冠脉血栓中发现大量嗜酸性粒细胞浸润。而HP可能通过参与炎症反应影响外周血嗜酸性粒细胞水平,减少的外周血嗜酸性粒细胞可能转移至冠脉内,进而参与血栓形成,导致急性心梗发生。
就颈部动脉粥样硬化而言,许多研究提示,Hp 感染可能是通过炎症反应、影响血脂代谢或同型半胱氨酸水平等途径使颈动脉内膜增厚,进而发展为颈动脉粥样硬化。
有研究显示,根除Hp后,患者血脂、同型半胱氨酸水平明显降低,颈动脉斑块治疗效果也得到显著提高。
总而言之,我国是Hp感染的高发国家,不论是保护心血管还是胃,都应该积极进行防治Hp感染。
目前推荐铋剂四联(PPI+铋剂+2种抗菌药物)作为主要的经验性治疗根除Hp方案(表1)。
表1 推荐的幽门螺杆菌根除四联方案中抗生素组合、剂量和用法
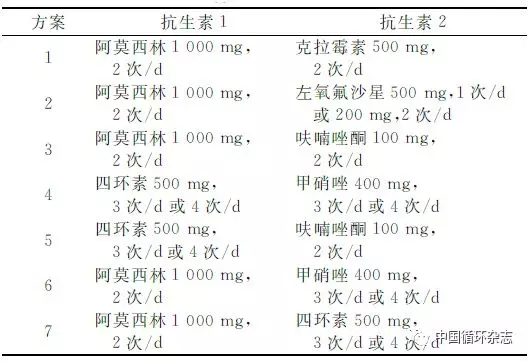
注:标准剂量(质子泵抑制剂+铋剂;2次/d,餐前0.5 h口服)+2种抗生素(餐后口服)。标准剂量质子泵抑制剂为艾斯奥美拉唑20 mg、雷贝拉唑10 mg(或20 mg)、奥美拉唑20 mg、兰索拉唑30 mg、泮托拉唑40mg、艾普拉唑5 mg,以上选一;标准剂量铋剂为枸橼酸铋钾220mg(果胶铋标准剂量待定)。
原始出处:
董雪珊,陈子龙,范文欣,等. 幽门螺旋杆菌感染与颈动脉内膜中层厚度相关性的Meta分析. 中国循环杂志,2018, 33: 366-.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#粥样硬化#
28
学习了.谢谢
50
学习了.谢谢
56
学习了.
56
学习
45
学习一下谢谢
59
HP感染在心梗发生中扮有一定角色.首都医科大学附属北京天坛医院王德昭.陈蕾蕾等对662例冠心病患者进行的研究显示.急性心梗患者中有46.5%的人感染了HP.显著高于稳定性心绞痛患者的38.4%.
26
不错的文章值得拥有
27