Clin Cancer Res:谢丹团队发现食管癌恶性进展的新分子通路
2017-04-29 佚名 华南肿瘤学国家重点实验室
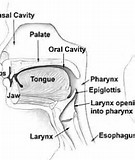
食管癌是我国最常见的头颈部恶性肿瘤之一,手术联合放化疗是该肿瘤的主要治疗模式。临床上,由于食管癌极高的复发和转移率,导致该疾病的预后较差。因此,深入探讨食管癌复发转移的生物学机制,寻找有效预测疾病复发和转移的分子指标,将显着提高食管癌患者的治疗效果和预后。日前,由谢丹教授团队联合中山大学附属第一医院叶升教授团队,在前期发现新癌基因PITX2 促进食管癌放化疗抵抗和不良预后的基础上,对 PITX2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新分子#
32
食管癌恶性进展的新分子通路。
58
继续学习。
61
#食管#
32
学习了,谢谢分享。
72
不错
58
期待!
74