JCC: CXCR3配体可以作为克罗恩病患者术后复发的生物标志物
2021-11-03 MedSci原创 MedSci原创
炎症性肠病是一种持续或反复发作的疾病,是起始于胃肠道黏膜的炎症。炎症可出现在消化道的任何部分,从口腔到肛门,例如直肠或小肠。
克罗恩病 (CD) 是一种慢性炎症性肠道疾病,大约三分之一的CD患者在确诊后五年内需要进行肠切除术,虽然“生物时代”已经到来,手术率显着下降,但肠切除术仍然是CD的主要治疗手段。CD患者疾病复发通常发生在新的末端回肠,并可以使用Rutgeerts 评分进行复发的判断,该评分已被证明可以预测重要的临床结果包括临床复发和需要进一步手术的需求。评估CD患者术后疾病复发的替代方法包括临床评估、CRP 和粪便钙卫蛋白检测,但是每种方法都有其局限性,本项研究旨在确定与CD复发相关的血液的生物标志物。

本项研究把接受回结肠切除术(ICR)的CD患者纳入了最后的分析,在术后结肠镜检查中获得患者的血清样品。多重免疫分析用于分析92种炎症相关蛋白 (Olink Proteomics)与CD疾病的相关性。
本项研究总共获得 213 名患者的 276 次结肠镜检查的数据。从手术到第一次和第二次结肠镜检查的中位时间分别为7和19个月。疾病复发在第一次和第二次结肠镜检查中很明显。在与 Rutgeerts 评分显着相关的 14 种蛋白质中,CXCL9 和 MMP1 的预测术后复发的能力最强。在使用抗TNF的患者中,CXCL9 和 CXCL11与 Rutgeerts 评分的相关性最强。两者都是CXCR3配体。与单独的C反应蛋白相比,将鉴定的蛋白质纳入 ROC 分析提高了鉴定疾病复发的能力。单细胞转录组数据表明先天免疫细胞是已鉴定蛋白质的主要来源。
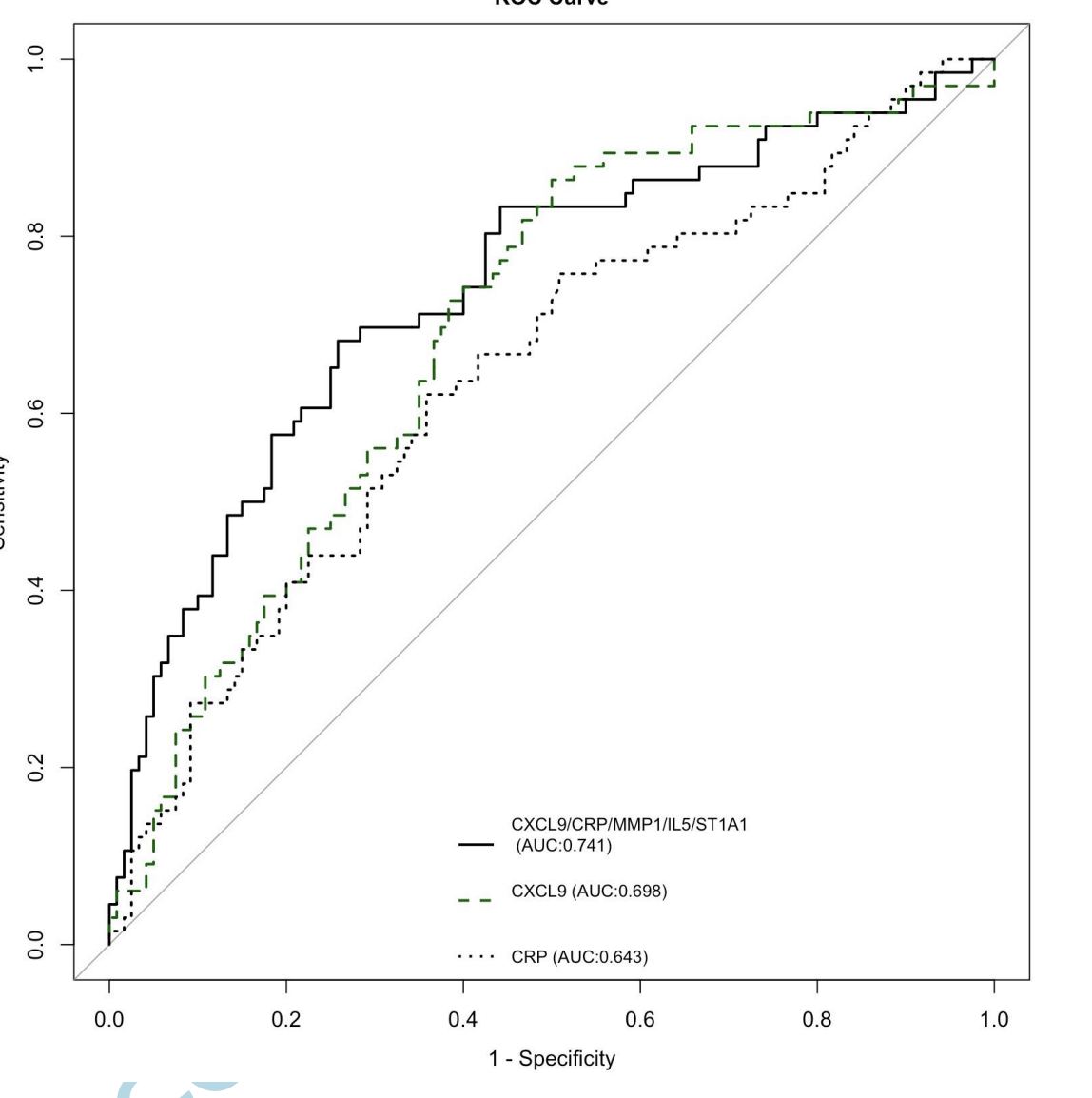
本项研究确定了许多新的候选蛋白质生物标志物与CD患者术后复发有关,特别是回结肠切除术后CD的复发有关。其中,CXCR3 配体与ICR后CD复发最有相关性。本项研究证实基于血液的候选生物标志物可能有助于识别CD的复发。
原始出处:
Margaret Walshe. Et al. A role for CXCR3 ligands as biomarkers of post-operative Crohn’s disease recurrence. Journal of Crohn's and Colitis.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#标志物#
42
#术后复发#
48
#生物标志#
36
#生物标志#
30
#克罗恩病#学习
122
学习新知识
87