JAHA:慢性肾脏病和非ST段抬高型心肌梗死患者的有创与药物治疗比较
2022-06-18 MedSci原创 MedSci原创
与药物治疗相比,有创治疗与较低的死亡率和主要不良心血管事件相关,但在NSTEMI-CKD患者中,院内并发症的增加最少,这表明应为NSTEMI-CKD患者提供有创治疗。
鉴于CKD患者手术并发症的风险增加,有创治疗与药物治疗在非ST段抬高心肌梗死(NSTEMI)和晚期慢性肾病(CKD)患者中的作用尚不明确。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员旨在比较NSTEMI-CKD患者的有创治疗与药物治疗对患者的临床结局。
研究人员使用来自2016年至2018年期间全国再入院数据库的第十修订版国际疾病分类(ICD-10-CM)代码确定了入院的NSTEMI和3、4、5期CKD以及终末期肾病患者。患者被分层接受有创和药物治疗。该研究的主要结局是死亡率(住院和出院后6个月),该研究的次要结局是院内术后并发症(需要透析的急性肾损伤、大出血)和出院后6个月的安全性和主要不良心血管事件。
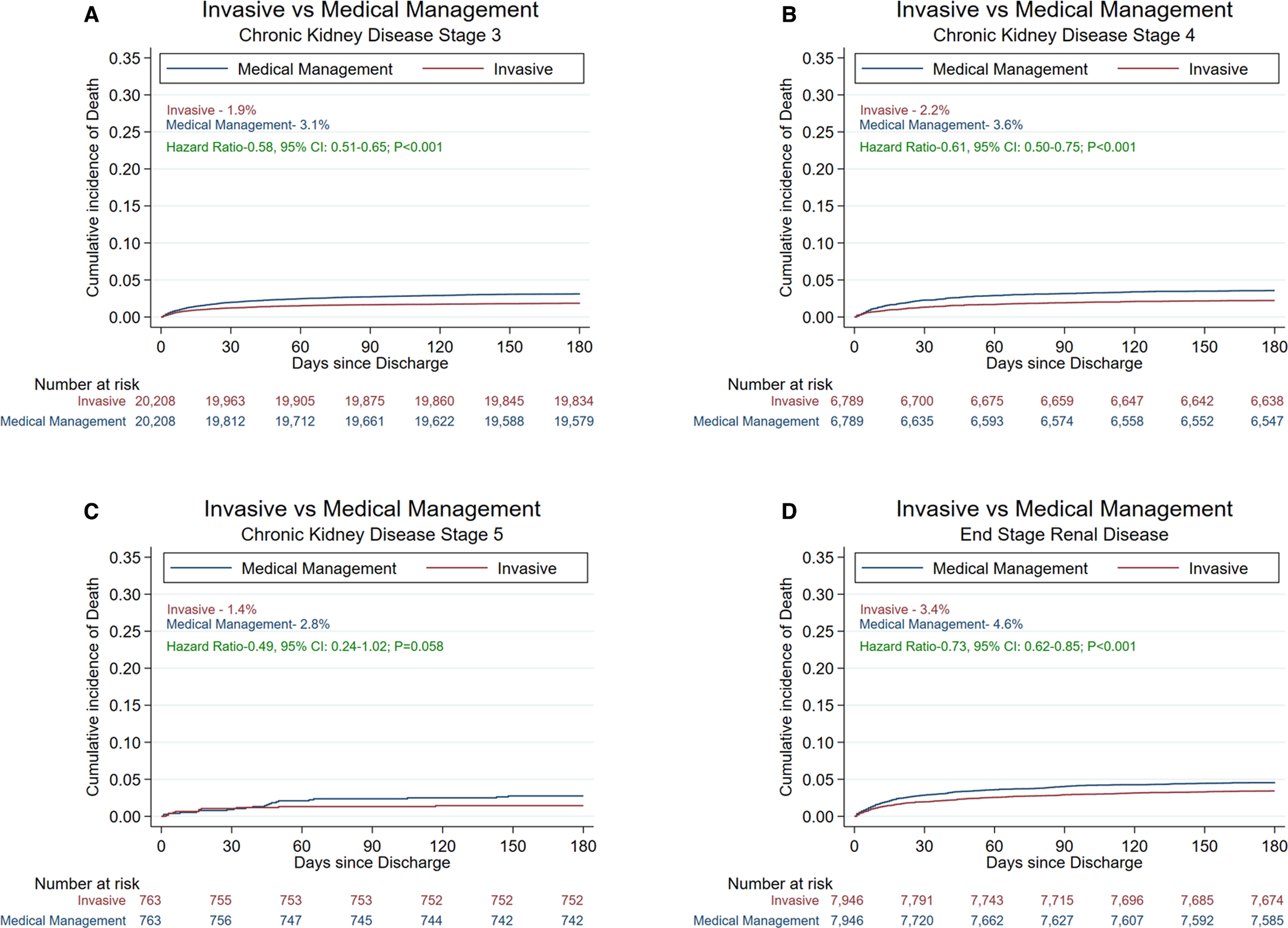
在141052名NSTEMI-CKD患者中,85875名(60.9%)患者接受了有创治疗,而55177名(39.1%)患者接受了药物治疗。在倾向评分匹配的队列中,有创治疗与较低的住院(3期CKD:比值比[OR]为0.47[95%CI为0.43-0.51];P<0.001;4期CKD:OR为0.79[95%CI为0.69-0.89];P<0.001;5期CKD:OR为0.72[95%CI为0.49-1.06];P=0.096;终末期肾病:OR为0.51[95%CI为0.46-0.56];P<0.001)和6个月死亡率相关。有创治疗与较高的院内术后并发症相关,但在出院后安全结局方面没有差异。与药物治疗相比,在所有CKD组中,有创治疗与6个月时主要不良心血管事件的风险较低相关。
由此可见,与药物治疗相比,有创治疗与较低的死亡率和主要不良心血管事件相关,但在NSTEMI-CKD患者中,院内并发症的增加最少,这表明应为NSTEMI-CKD患者提供有创治疗。
原始出处:
Monil Majmundar.et al.Invasive Versus Medical Management in Patients With Chronic Kidney Disease and Non–ST‐Segment–Elevation Myocardial Infarction.JAHA.2022.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.025205
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#非ST段抬高#
53
#非ST段抬高型心肌梗死#
48
#非ST段#
53
#非ST段抬高型#
42
#AHA#
39
#ST段抬高#
53
#慢性肾脏#
53
#ST段#
47
#治疗比较#
38