胸腔镜下瓣膜成形及置换术
2017-02-25 佚名 搜狐
心脏瓣膜病是由多种原因引起的单个或多个瓣膜结构的功能或结构异常,导致瓣某狭窄和(或)关闭不全,患者表现为心慌、气促,治疗时需采取瓣膜成形手术和置换手术。
心脏瓣膜病是由多种原因引起的单个或多个瓣膜结构的功能或结构异常,导致瓣某狭窄和(或)关闭不全,患者表现为心慌、气促,治疗时需采取瓣膜成形手术和置换手术。
心脏瓣膜成形手术-上海远大心胸医院
传统瓣膜成形手术是指在全身麻醉的情况下操作,切口在胸部正中(胸骨),长20cm左右,在体外循环下进行瓣膜修复,主要修复方式包括瓣叶部分切除修补术、瓣膜或键索粘连分离术、腱索缩短或移植术,人造瓣环行瓣环缩小及瓣环畸形矫治术等,故又称为“瓣膜综合成形术”。不同心脏瓣膜病,其修复成形的方法也不一样。
心脏瓣膜置换手术-上海远大心胸医院
当患者心脏瓣膜结构受损严重时,瓣膜成形手术已无法修复,此时需要切除已遭病变损坏的瓣膜,然后将一种人工制成的瓣膜通过手术缝合的方法,固定在原来的瓣膜位置上,人工心脏瓣膜将 替代原来心脏瓣膜的功能,这就是瓣膜置换手术。
哪些患者适合瓣膜置换手术?主要根据病人心脏瓣膜的损坏程度。凡是瓣膜病变严重又无法做成形手术的患者,只要全身情况允许都应争取实施瓣膜置换手术,病人的年龄没有 限制。目前瓣膜置换术约占全部瓣膜手术的90%。
人工瓣膜是选择机械瓣还是生物瓣好?-上海远大心胸医院
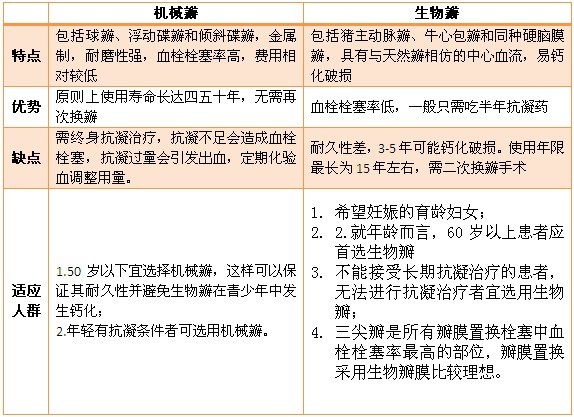
瓣膜置换手术可选择机械瓣也可选择生物瓣,他们各有优缺点,可根据患者年龄、职业、体力、精神状态和病情需要(患者的心肌情况和患者能否接受长期的抗凝治疗)以及患者对瓣膜选择的意见综合考虑。目前机械瓣膜置换占总数的90%,生物瓣膜置换占10%。
生物瓣与机械瓣的优缺点比较
瓣膜置换手术的相对禁忌症-上海远大心胸医院
风湿活动未被控制或控制不足3个月;
心力衰竭合并心肌缺血损坏者如主动脉瓣狭窄的晚期病人,心功能有所改善,仍争取手术;
肝、肾功能或全身情况太差而不能经受手术的患者;
细菌性心内膜炎病人已出现败血症并多处感染者不宜手术。
传统瓣膜成形及置换手术-上海远大心胸医院
传统的手术方式需要 劈开胸骨,手术结束时用钢丝合拢固定胸骨,其优点是显露心脏病变好,操作方便。但这种切口不仅易发生愈合不良裂开和胸骨畸形,钢丝终生遗留在胸骨,胸部X线检查检查时一目了然。而且手术切口大,皮肤疤痕呈蜈蚣样位于胸部前面正中,给患者,特别是女性患者的美观、社交与心理带来了严重的不良影响,如无法穿低领或开领衣服、自卑感等。虽然心脏病及时手术后绝大多数患者 可以像普通人一样正常的生活、学习和工作,但由于皮肤疤痕和胸骨内钢丝使其做过心脏大手术的事情显而易见,对患者的升学和就业非常不利。
胸腔镜下瓣膜成形及置换术-上海远大心胸医院
上海远大心胸医院特色治疗方法为 胸腔镜下瓣膜成形及置换手术,这种疗法在胸壁仅有三个1.5厘米左右的钥匙孔样小孔进行手术,病人创伤小,恢复快,手术安全,胸壁无大的切口而且美观。
胸腔镜技术被认为是自体外循环问世以来,是心脏外科领域里又一次重大技术革命,是现代微创心脏外科的代表性手术。与传统的手术相比,胸腔镜微创心脏外科手术具有以下优点:皮肤切口小(1-2cm),不切断肌肉,无骨骼损伤,创伤小恢复快,手术后疼痛轻,5-7天就可以出院,符合美容要求,费用低于传统心脏手术。基本上传统开胸手术能治疗的心脏瓣膜病变都能使用胸腔镜手术治疗。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







请问是如何做到不切断肌肉呢? 进入胸腔不需要切口吗?
39
#置换#
23
#胸腔镜#
27
#置换术#
34
#瓣膜#
30