山东省首例:经典Bentall术,牛兆倬教授团队成功完成院内INSPIRIS¹主动脉瓣膜首次临床应用!
2021-06-28 “Clinic門诊新视野”公众号 “Clinic門诊新视野”公众号
2021年4月27日,在武汉亚洲心脏病医院陶凉院长的指导下,青岛市市立医院牛兆倬教授心脏外科团队使用INSPIRIS[1]主动脉瓣生物瓣(以下简称INSPIRIS[1]),为一例70岁的主动脉瓣近中度
2021年4月27日,在武汉亚洲心脏病医院陶凉院长的指导下,青岛市市立医院牛兆倬教授心脏外科团队使用INSPIRIS[1]主动脉瓣生物瓣(以下简称INSPIRIS),为一例70岁的主动脉瓣近中度反流患者实施了经典的Bentall手术(又称“复合带瓣管道主动脉瓣和升主动脉置换术”),不仅成功完成了INSPIRIS[1]在本中心,乃至山东省的首次临床应用,同时在默契的团队合作中精彩展示了该款瓣膜独特的设计优势以及应用技巧。术后第一时间,《门诊》杂志记者现场采访牛兆倬教授,分享了新型INSPIRIS[1]的设计特点及临床应用中的自我体会。接下来,就让我们一同回顾术中的精彩瞬间及专家的自我观点与建议。

病例描述 | 近中度主动脉瓣关闭
不全、升主动脉夹层动脉瘤
患者女,70岁。心脏超声提示,主动脉瓣为三叶瓣结构,瓣膜增厚,开放可,舒张期见近中量中心性反流,主动脉瓣环平均直径25.5 mm;升主动脉及主动脉窦扩张,升主动脉平均直径55 mm,主动脉窦平均直径47 mm;E/A<0.8,Em降低,提示左室舒张功能轻度减低;EF为58%。
术前超声
综合上述评估结果,患者具备外科换瓣指征,拟行主动脉瓣置换术。在瓣膜类型选择方面,考虑到患者对生活质量要求较高及自身身体素质较佳等主客观因素,最终考虑为其植入集耐久性优异、血流动力学表现良好等多个优点于一身的爱德华INSPIRIS RESILIA[1]主动脉瓣膜一枚。
操作流程 | 有条不紊完成Bentall手术,
超声提示无主动脉瓣反流

术前准备:
将新型INSPIRIS生物瓣缝在人工血管上,成功制备带瓣管道。

术中操作:
(1)术中采取仰卧位,胸骨正中切口,采用上、下腔静脉插管和股动脉插管建立体外循环;首次心脏停搏液在切开升主动脉瘤后直接做左、右冠状动脉灌注,而后采用经冠状静脉窦持续或间断灌注冷血心脏停搏液;
(2)主动脉切口:先做升主动脉瘤纵切口,注意观察主动脉瓣,特别关注左、右冠状动脉开口的位置。然后在右冠状动脉开口上方2.0 cm,横行剪断升主动脉瘤下端的前半部,以充分显露主动脉瓣和右冠状动脉开口;
(3)置换主动脉瓣:完整剪除原有的病变瓣叶,并清除瓣环上可能存在的钙化组织等;用带垫片的缝线,连续缝合主动脉瓣环,缝合时一定要严密,以防术毕出血。最后将主动脉瓣环缝合线穿越带瓣管道的瓣环,逐一打结;
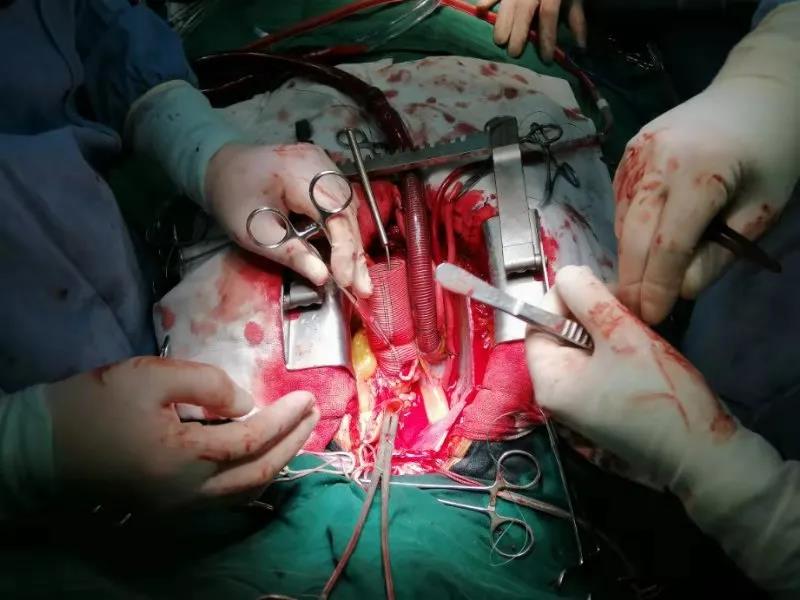
(4)左、右冠状动脉移植:行左、右冠状动脉开口与人造血管吻合;
(5)人造血管与升主动脉远端吻合:修剪带瓣管道至适当长度,人造血管的前半部较后半部长约1.5 cm,有利于吻合后无扭曲。用4-0聚丙烯线先行腔内连续缝合后壁左侧至右侧壁,再用另一端缝线连续腔外缝合侧壁和前壁;
(6)术毕在人造血管上插入排气针,头低位,开放主动脉阻断钳,充分排气后,缝合针孔出血。开放升主动脉,等待患者心功能恢复,待心率、血压平稳后停体外循环,最后关胸,结束手术。术后超声提示即刻跨瓣压差几乎为零,无主动脉瓣反流。
术后超声
术后点评 | INSPIRIS瓣膜,满足患者
对术后高质量生活的需求
牛兆倬教授:这是一位70岁、伴有主动脉瓣近中度关闭不全的老年女性患者,结合超声评估结果及现有指南推荐,外科主动脉瓣膜置换是其有效的治疗手段。此外,在术前沟通中,我们了解到该例患者对术后的长期生活质量要求较高,建议采取生物瓣膜置换。
而在众多外科生物瓣产品中,一款于去年12月份在中国大陆正式上市的新型INSPIRIS[1]主动脉瓣膜受到了本科室心脏外科医师的瞩目,团队成员一致认为该款瓣膜与患者的自身需求及术后良好预后的获得等极为契合。一方面,该例患者虽已年满70周岁,但身体状况良好,预期寿命较长;当前,临床中常用的生物瓣膜预期使用寿命仅为10-15年,而INSPIRIS[1]生物瓣作为一款新型干瓣,成功搭配了全新RESILIA组织,耐久性大幅提升、瓣膜使用时间显着延长,为患者后续高质量生活的保障提供了极大助力。另一方面,INSPIRIS[1]生物瓣开创性地引入了VFit可扩展瓣架技术,可为未来瓣中瓣介入疗法预留解决方案;INSPIRIS[1]生物瓣与TAVR技术实现“完美融合”,提供了患者全生命周期的解决方案,即使随着年龄的增长患者出现了生物瓣膜毁损的问题,也可通过瓣中瓣技术较为顺畅地再次植入一枚瓣膜,使患者术后无需终生抗凝成为可能。基于上述应用优势,我院团队积极与该患者进行沟通,最终患者选择了INSPIRIS[1]新一代生物瓣。
值得注意的是,本例患者除具备主动脉瓣关闭不全特征之外,同时胸主动脉检测提示升主动脉动脉瘤且主动脉窦存在明显扩张,单纯主动脉瓣置换手术并非最佳治疗策略,而应采取经典的Bentall手术。在国内知名心外科专家陶凉院长的指导下,本团队首先将新型INSPIRIS[1]生物瓣缝在人工血管上,成功制备带瓣管道。随后,在体外循环条件下,先后经过主动脉切口、置换主动脉瓣、左右冠状动脉移植、人造血管与升主动脉远端吻合等步骤,十分顺利地完成了整个Bentall手术;其中,在主动脉瓣置换操作中,本团队特别采用了连续缝合法,不仅对合整齐、严密,闭合、止血效果良好,而且INSPIRIS[1]生物瓣特别改良的缝合环设计,使得置针更为轻松,手术操作十分顺畅。术后即刻超声检查显示,跨瓣压差几乎为零,无主动脉瓣反流,整体效果令人非常满意。
作为一种被植入体内的人工异物,瓣膜产品的耐久性、血流动力学表现等特征,往往是影响患者生活质量、预期寿命的重要因素,一直备受广大临床医师以及患者群体的关注与讨论;相较于其他类型的人工瓣膜产品,INSPIRIS[1]生物瓣当属一款在理念或设计上十分前沿的主动脉瓣膜,代表了当前瓣膜领域的较高水准,特别适合于对生活质量要求高、预期寿命较长的一类患者,而本次院内INSPIRIS[1]生物瓣首次临床应用的优秀表现,也进一步验证了该款瓣膜的种种优异性能。INSPIRIS作为一款集卓越耐久性、优异血流表现、植入体验升级等多种优点于一体的主动脉瓣膜,其未来市场需求十分强劲;相信通过国内应用范围的不断拓展,更多瓣膜性心脏疾病患者可从中获益!
本院心外科作为山东省临床重点专科,自创建以来始终秉承“以患者为中心、全方位提升医疗服务质量”的宗旨,不断开拓创新,在加强业务学习、提升自身技术水平的同时,始终致力于把握疾病诊疗先进技术、积极引进性能优异的新型人工心脏瓣膜等手术耗材,在冠心病、大血管、心脏瓣膜病等亚专科建设方面作出了不懈努力,取得了“病种覆盖全、高难度手术成功率高且手术量大、术后并发症发生率低”等一系列骄人的成绩。当前,本科室不仅能够熟练完成非体外循环下及体外循环辅助下冠脉搭桥手术的操作及术后处理,同时可常规开展心脏瓣膜置换手术,在心脏瓣膜修复手术尤其是风湿性瓣膜修复技术、重症瓣膜疾病治疗等方面均积累了丰富的经验。未来,本中心将继续提升专业技术水平,为省内患者带来更好的诊疗体验,推动区域医疗水平不断向前发展。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#山东省#
41
#临床应用#
36
#ALL#
26
#主动脉瓣#
32
#主动脉#
41
#瓣膜#
29