Science Advances :触发感染性休克的新分子信号
2017-05-04 MedSci medicalxpress
来自KAIST Seyun Kim的研究团队报道了细胞信号转导网络在调节先天免疫反应的过程中,如酶IPMK(肌醇多磷酸盐多激酶)对肌醇生物合成代谢的关键作用。 该研究与首尔国立大学的Rho Hyun Seong教授合作完成。文章第一作者、生物科学系的博士研究生尤妮哈·金(Eunha Kim)进行了一系列细胞、生化和生理学的实验,寻找巨噬细胞中IPMK酶的新功能。这项研究结果发表在4月21日的《科
来自KAIST Seyun Kim的研究团队报道了细胞信号转导网络在调节先天免疫反应的过程中,如酶IPMK(肌醇多磷酸盐多激酶)对肌醇生物合成代谢的关键作用。
该研究与首尔国立大学的Rho Hyun Seong教授合作完成。文章第一作者、生物科学系的博士研究生尤妮哈·金(Eunha Kim)进行了一系列细胞、生化和生理学的实验,寻找巨噬细胞中IPMK酶的新功能。这项研究结果发表在4月21日的《科学进展》上。
Kim教授的研究小组已经对各种肌醇代谢物和他们的生物合成代谢进行了几年的研究,并在细胞生长和能量平衡的控制中,对IPMK(肌醇多磷酸盐多激酶)的信号行为进行了多边识别。
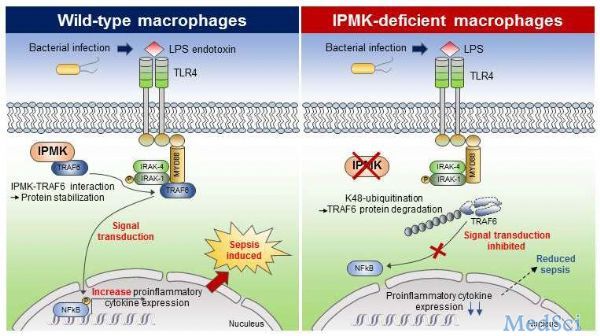
该研究表明,当微生物脓毒性休克和内毒素激发时,巨噬细胞中IPMK酶的特异性缺失可显着降低小鼠的炎症水平并提高小鼠的存活率。这表明了IPMK酶在调节先天炎症反应中的作用,反应与宿主防御致病性细菌感染直接相关。
该小组进一步发现IPMK酶直接与TRAF6蛋白结合,TRAF6蛋白是免疫信号传导的关键蛋白,从而保护TRAF6蛋白免于参与蛋白质降解的泛素化反应。此外,Kim等人通过使用能够特异性干扰IPMK酶和TRAF6蛋白在巨噬细胞中结合的短肽,成功验证了IPMK依赖性免疫控制。
本研究揭示了IPMK酶在先天免疫信号网络微调中的一个新功能,提出了一种新的治疗方法,用于治疗严重的疾病,如神经炎症、2型糖尿病,以及由不受控制的宿主免疫反应产生的多菌败血症。研究获科技部、ICT和未来计划项目资助。
原文出处: Eunha Kim et al, Inositol polyphosphate multikinase promotes Toll-like receptor–induced inflammation by stabilizing TRAF6, Science Advances (2017).
此文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













科研
58
#新分子#
30
#感染性#
22
学习了,谢谢作者分享!
59
新信号通路发现
76
#SCIE#
25