JNS:多节段硬膜外脓肿的微创手术方法
2013-06-13 JNS dxy
简介:本文阐述了多节段脊髓硬膜外脓肿(SEA)的一种微创治疗方法,通过在病变节段置入管型牵开器引流脓肿成功治愈3例病例,所有病例术后预后结果良好。 脊髓硬膜外脓肿(SEA)是较为严重的感染,约占住院患者的2/10000*年。SEA可以出现急性神经症状,即使得到有效的治疗,仍具有较高的致残率和致死率。SEA脓肿通常沿脊髓节段延伸,最常累及胸段脊髓,其次是腰段。 多节段的SEA是目前临床治疗的难点
简介:本文阐述了多节段脊髓硬膜外脓肿(SEA)的一种微创治疗方法,通过在病变节段置入管型牵开器引流脓肿成功治愈3例病例,所有病例术后预后结果良好。
脊髓硬膜外脓肿(SEA)是较为严重的感染,约占住院患者的2/10000*年。SEA可以出现急性神经症状,即使得到有效的治疗,仍具有较高的致残率和致死率。SEA脓肿通常沿脊髓节段延伸,最常累及胸段脊髓,其次是腰段。
多节段的SEA是目前临床治疗的难点,对这类疾病患者,传统的手术治疗方法是广泛暴露病变累及节段行脓肿切排。该方法的缺点在于:术后潜在的脊柱稳定性破坏有可能导致后期患者出现脊柱畸形和不稳定;同时因该手术暴露较大,存在术中手术时间较长,出血较多,术后疼痛增加,较长的住院和康复时间等缺点。近期有学者通过一种微创的置管引流脓肿法治疗脊髓硬膜外感染,同时能较好的保持脊柱节段稳定性。
本文报道一种改良的治疗多节段SEA的手术方法,通过微创手术方法置入一个管型牵开器行广泛的硬膜外脓肿引流,同时联合药物治疗成功治愈3例多节段SEA。该方法应用前提是所有节段脓肿均为液性,具体在影像学上表现为T1加权低信号;同时积液处于硬脊膜鞘膜外。
手术方法:
患者达成全麻后俯卧位,通过术前的MRI片准确的定位患者的脓肿节段,通过C臂机进行确认并确定进针点。若患者存在多节段脓肿,则可行2个或2个以上的旁正中入路切口,切口分别靠近脓肿的头端和尾端,若脓肿较大,则在脓肿中间端再开一皮肤切口;若患者脓肿节段较少,则在脓肿中间开口。牵开皮肤和筋膜,置入管型扩张器(METRx, Medtronic Sofamor Danek)。使用高速钻头和Kerrison咬骨钳行办椎板切除术。暴露黄韧带,切除,而后在扩开的切口内放置18mm直径的引流管,将自行流出的脓液吸除,而后在硬膜外腔隙中放置小的带角度的脑垂体吸引器(small angled pituitary suction tips),链接负压引流装置,大量冲洗,直至所有脓肿被排出。术后冲洗排出的脓液行细菌培养以指导患者术后的抗生素选择。若有需要,术者可以使用微创带角度的镜头观察脊柱附件和脓肿清除情况。术后患者接受4-6周的抗生素治疗,至患者的CRP及ESR等指标回归正常。而后行MRI评估患者的脓肿治疗情况。
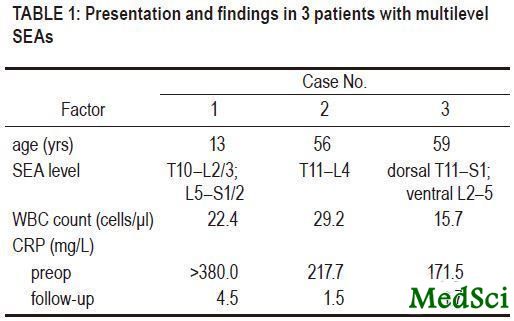
通过上述方法,研究者治愈了3例多节段SEA患者,相关数据如表1所示。现将治愈的病例介绍如下。
表1:3例SEA患者相关统计数据
病例1:
13岁男性,腰背部,腹部疼痛,排尿困难1周。体格检查发现患者胸椎及肋椎关节触痛,就诊时患者因疼痛无法行走,但检查无明显感觉或运动损伤。血常规检查提示WBC 22.4个/ul,CRP>380mg/l,ESR97mm/hour。影像学检查提示脊椎椎管后方从T10节段-L2-3节段广泛的硬膜外脓肿,另有一个从L5-S1-2较局限脓肿(图1左)。治疗时在患者的右侧T12节段、L2-3节段、L5-S1节段行旁正中长约18mm切口,其余操作方法同之前手术技术。细菌培养结果提示金黄色葡萄球菌。患者术后行4周万古霉素+氯林可霉素治疗,出院时患者CRP及ESR下降至正常水平。术后6月患者的MRI检查发现脓肿完全消退(图1右),术后患者恢复良好。

图1:矢状位MRI图。左:术前腰椎T1增强提示后方广泛脓肿;右:术后腰椎T1增强提示脓肿消除
病例2:
56岁男性,既往有糖尿病史,血糖控制不佳,腰痛及下肢枪击样神经痛根痛1周。体检时发现患者双髋部运动功能减弱,其余无明显神经症状。MRI检查提示T11-L4节段硬膜外脓肿,硬脊膜挤压明显(图2)。在L1-2、L3节段行置管引流。术后抗感染治疗,炎症指标好转后出院。术后6月随访,CRP正常,无明显临床症状,因患者最后失随访,未行MRI检查。

图2:术前矢状位MRI T1增强相提示T11-L4脓肿形成。
病例3:
59岁男性,既往有右前臂蜂窝织炎和糖尿病病史,血糖控制不佳,近期出现尿路感染,菌血症,同时出现间歇性的腰背部疼痛。WBC为15.7/ul,CRP171.5mg/l,MRI检查提示患者T11-L2节段硬脊膜背侧巨大脓肿,在L1节段行切口放置引流管。术后细菌培养提示金黄色葡萄球菌,行抗感染治疗4周,随后随访过程中未出现症状复发,炎症指标回归正常。术后2月复查MRI,脓肿完全消失,图3。

图3:矢状位MRI图。左:术前胸腰椎T2增强提示T12-L2后方广泛脓肿;右:术后腰椎T1提示脓肿消除
讨论:
目前报道SEA治疗方法的文献较多,从经皮穿刺脓液抽吸到多节段椎板切除+脓肿切排等。经皮脓肿穿刺引流适用于后方SEA不伴有神经症状者,其潜在的危险是可能导致脓肿扩散至其他部位。在一项由Reihsaus等完成的对915例SEA患者的Meta分析中总结认为目前椎板切除术是大部分医生的推荐术式,一旦患者确诊为SEA,应当尽早实行手术治疗。但是多节段的椎板切除术,特别是在儿童和成人中,可能导致后期的脊柱畸形。椎板切除术后的脊柱不稳定决定因素较多,包括年龄,关节突关节切除范围,椎板切除数目,部位及术前患者脊柱排列等均可能对术后患者的脊柱稳定性造成影响。
有些学者建议在能保存脊柱稳定性的前提下尽可能的切除多的椎板以获得脓肿的彻底清除。然而,这在多节段的SEA患者中显然并不现实。同时过大的手术范围可诱发如失血,败血症,心肺,肾脏等多种系统性疾病。此外,广泛剥离脊柱旁肌肉和脊柱可以限制术后腰椎运动和恢复。因此有些学者建议,椎板切除应当控制在3节段内,对多节段脓肿,可间隔一个或多个节段行椎板切除。也有学者建议腰椎脓肿患者通过椎板间入路行椎板间黄韧带切除术进行治疗,但因为胸椎内解剖结构的关系,该方法应用更为困难。
近期已有学者开创了微创引流治疗广泛SEA的方法。这些方法的基本原理是行有限的椎板切除或椎板切开术,将柔软的橡胶导管放置入硬膜后间隙内,行脓肿冲洗和引流。本文介绍的方法和上述原理类似,但是不同点在于,在暴露椎板时应用了微创的管道牵开器,在不同阶段行牵开器下半椎板切除和脓肿引流,该方法减少了大切口范围时周围组织的感染概率,不仅允许对脓肿物质进行直视下引流,而且允许对硬膜外腔隙进行冲洗。
若患者的脓肿延伸至前方,可使用钝性的神经拉钩牵开神经,将细小柔软的硅胶管放置在前方使用抗生素溶液进行脓肿清除和冲洗。在放置冲洗管道是需要注意材质柔软,以防止穿透硬膜。该方法可以减少椎板切除的范围,减少术中失血量及术后切口感染率,加快术后恢复速度;因脊柱稳定性得到较好的维持,后期出现脊柱后凸畸形的可能性降低。但同时需要说明的是:该技术方法只能应用于脊柱脓肿为液性,脓肿居于脊柱硬脊膜后方的患者中。若患者存在蜂窝织炎或炎性肉芽形成,则推荐行传统开放手术治疗。
结论:
通过微创管型牵开器置入系统行半椎板切除,硬膜外脓肿引流治疗胸腰椎脓肿安全有效,可避免多节段椎板切除所带来的缺点,值得推荐。

Minimally invasive treatment of multilevel spinal epidural abscess.
AbstractThe use of minimally invasive tubular retractor microsurgery for treatment of multilevel spinal epidural abscess is described. This technique was used in 3 cases, and excellent results were achieved. The authors conclude that multilevel spinal epidural abscesses can be safely and effectively managed using microsurgery via a minimally invasive tubular retractor system.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#硬膜外#
37
#微创手术#
26
#微创#
27
#手术方法#
29
#脓肿#
26