Neurology:颈动脉斑块炎症的PET显像与5年再发卒中的预测
2021-10-19 Naomii MedSci原创
斑块炎症相关的18FDG摄取改善了5年复发性同侧缺血性卒中的鉴别。将斑块炎症添加到目前的选择策略中,可能针对最有可能从颈动脉血运重建中获得晚期和早期益处的患者。
颈动脉狭窄在15%-20%的缺血性中风患者中被发现,与其他中风亚型相比,颈动脉狭窄与早期复发的风险更高。炎症在动脉粥样硬化斑块的发展和不稳定至关重要。临床病理研究表明斑块炎症、斑块不稳定的形态特征和中风复发之间存在关联。抗炎治疗可预防冠心病患者的复发血管事件,包括中风。18FDG-PET是一种经过验证的非侵入性成像技术,可用于炎症相关的斑块代谢,并与切除的人颈动脉斑块的炎症组织学证据相关。
目前还没有关于症状出现后不久测量的颈动脉斑块炎症与中风复发和其他血管事件的晚期风险之间的关系的数据。通过研究PET在较长的时间间隔识别高危患者,这对颈动脉血运重建术(旨在预防晚期卒中复发)的患者选择有重要的潜在意义。近日,有研究人员对3项前瞻性队列研究中的个体患者数据进行了综合分析,探讨18F-脱氧葡萄糖(18FDG)-PET检测颈动脉斑块炎症是否与晚期(5年)再发卒中有关。

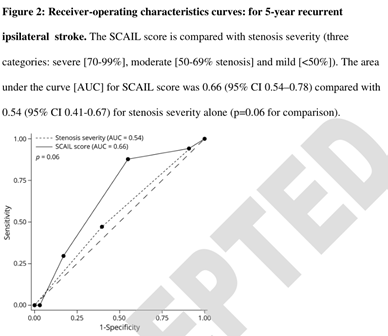
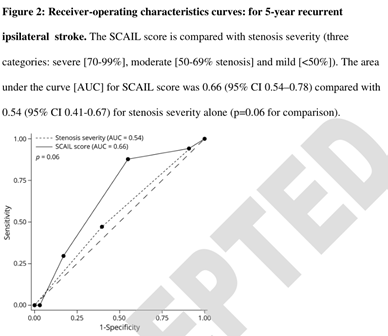
研究人员用统一的研究方法对3项前瞻性研究进行了参与者数据汇集分析。符合条件的患者有近期不严重(改良Rankin评分≤为3)、缺血性卒中/短暂性脑缺血发作和同侧颈动脉狭窄(50-99%)。受试者在入组后14天内接受颈动脉18FDGPET/CT血管造影检查。18FDG的摄取以症状性斑块轴向最热层面的最大标准摄取值(SUVmax)表示,并计算了先前证实的症状性颈动脉粥样硬化性炎症管腔狭窄(SCAIL)评分,该评分结合了狭窄严重程度和18FDG摄取的测量。主要结果是PET成像后5年内复发的同侧缺血性卒中。

- 183例符合条件的患者中,181例患者完成随访(98.9%)。中位随访时间为4.9年(四分位数范围3.3-6.4年,累计随访期901.8病人*年)。
- PET显像后,17例5年后再发同侧缺血性卒中(复发率9.4%,95%可信区间5.6~14.6%)。
- 基线斑块SUVmax的独立预测在调整了年龄、性别、颈动脉血运重建、狭窄严重程度、NIHSS评分和糖尿病后5年内同侧复发中风(调整后的HR为1.98;95%CI为1.10-3.56,p=0.02,每增加1g/mL SUVmax)。
- 在多变量Cox回归分析中,SCAIL评分可预测5年内同侧卒中(调整后的HR值为每增加1分2.73分;95%CI为1.52-4.90分,p=0.001)。
斑块炎症相关的18FDG摄取改善了5年复发性同侧缺血性卒中的鉴别。将斑块炎症添加到目前的选择策略中,可能针对最有可能从颈动脉血运重建中获得晚期和早期益处的患者。
文献来源:https://n.neurology.org/content/early/2021/10/05/WNL.0000000000012909.long
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#Neurol#
42
#PE#
39
#颈动脉#
45
#颈动脉斑块#
37
#斑块#
33
#PET#
30