NEJM:真恐怖!结肠息肉切除术致医源性穿孔--案例报道
2015-11-19 chenshuo译 MedSci原创
女性,65岁,经结肠镜下行手术切除结肠内息肉,术后转运到急诊科进行进一步的治疗。 当该女患者苏醒过来时,表现出强烈的痛苦状并伴有大汗不止。
女性,65岁,经结肠镜下行手术切除结肠内息肉,术后转运到急诊科进行进一步的治疗。
当该女患者苏醒过来时,表现出强烈的痛苦状并伴有大汗不止。
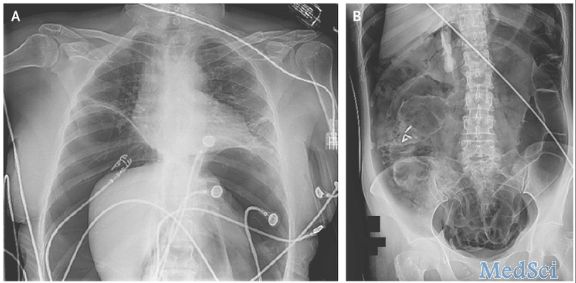
行胸部和腹部平片检查发现了大量的气体和腹腔内容物,膈下腹部呈巨大的张力(如图A和图B)。
随后,该患者再次被送往手术室,接受开腹减压(可点击原始链接观看视频)和楔形切除矫正升结肠医源性穿孔。
术后第三天,病人恢复良好顺利出院。
Haytham M.A. Kaafarani et al.Tension Pneumoperitoneum.NEJM.2015November 19, 2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









这个居然发了新英格兰。
76
肠镜并发症,内镜医生的噩梦
71
#切除术#
28
不错,赞一个
118
这篇文章有一定深度
119
是一篇不错的文章
116
值得临床关注
140
这么典型
47
值得关注
80
典型案例
96