袁响林教授:《CSCO胃癌诊疗指南》免疫治疗更新尽显前沿循证
2020-08-19 医学界 医学界
近日,《2020中国临床肿瘤学会(CSCO)胃癌诊疗指南》(以下简称“指南”)正式对外发布,今年指南的重点更新内容将成为未来临床治疗的风向标。
近日,《2020中国临床肿瘤学会(CSCO)胃癌诊疗指南》(以下简称“指南”)正式对外发布,今年指南的重点更新内容将成为未来临床治疗的风向标。
对此,医学界有幸邀请到华中科技大学同济医学院附属同济医院的袁响林教授,对本次指南更新中关于胃癌免疫治疗的亮点内容进行分析和展望。
免疫治疗推荐力求精准
整体上,此次指南更新对分子病理检测、放疗、化疗、免疫治疗等几大内容均做出了调整。其中,晚期转移性胃癌的免疫治疗部分将中国目前唯一获批晚期胃癌适应症的免疫肿瘤药物纳武利尤单抗作为单药推荐,且推荐等级相较既往单药PD-1单抗进一步提升,被列为I级推荐,1A类证据,用于晚期转移性胃癌的三线治疗,成为关注焦点之一。
此前,2018年指南首次将PD-1单抗纳入指南,列为III级推荐,1A类证据;2019年升级为II级推荐,1B类证据;今年指南对于免疫治疗的推荐更为细致,首次将免疫治疗以具体药品取代全品类进行详细推荐。
事实上,精准推荐也是进一步规范临床治疗的方式之一。考虑到PD-1单抗药物种类众多,各个药物之间存在疗效差异、批准的适应症也不同;因而,指南的推荐也会注重临床合理用药的要求。袁响林教授也在解读中强调,在实践中应尽可能地根据获批适应症来选择药物。
ATTRACTION-2研究结果显优效
袁响林教授谈道,胃癌的三线治疗在临床中很重要,但药物仍比较匮乏。此前的I级推荐仅有阿帕替尼。如今,新加入的纳武利尤单抗作为一项不受CPS评分限制的I级推荐,可能会彻底改变胃癌三线治疗的格局。这也是此次指南更新最重要的变化之一。
他指出,这项推荐主要以ATTRACTION-2研究结果为依据。ATTRACTION-2研究是全球首个启动的胃癌免疫治疗临床试验。研究共纳入493例东亚(日本、韩国和中国台湾)晚期胃癌患者,接受纳武利尤单抗或安慰剂用于三线及以上治疗。3年随访结果显示纳武利尤单抗降低了38%的死亡风险(HR 0.62,P<0.0001)。
纵览研究的生存曲线,纳武利尤单抗组:
- 1年OS率达到27.3%(安慰剂组为11.6%)
- 2年OS率为10.6%(安慰剂组为3.2%)
- 3年OS率为5.6%(安慰剂组为1.9%)
整体生存率是安慰剂组的2-3倍,可以明显看到免疫治疗的“生存长尾”。
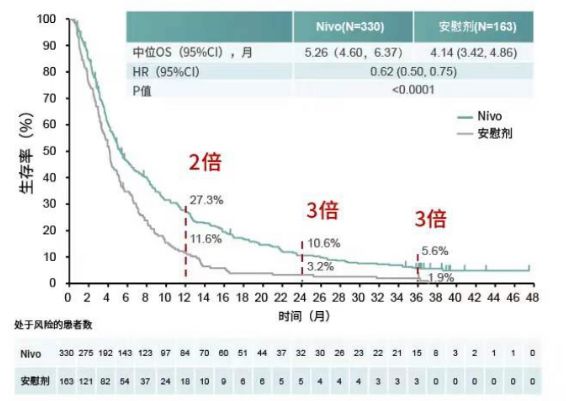
图1 ATTRACTION-2研究的3年OS结果
此外,亚组分析显示,纳武利尤单抗组有9.7%患者取得完全缓解(CR)/部分缓解(PR),这些患者的中位OS达到了26.68个月,超过了2年。相比之下,对照组没有患者取得CR/PR。
中国人群明确获益
在中国,约80%的胃癌患者确诊时已是进展期3,预后不理想。尽管晚期胃癌的治疗,尤其是晚期后线治疗,难度极大,但有效的治疗手段对数量庞大的患者而言却非常重要。
ATTRACTION-2研究的中国台湾亚组人群结果证明,纳武利尤单抗可为三线及后线治疗的中国晚期胃癌患者带来显著的生存获益。纳武利尤单抗组降低了51%死亡风险(OS的HR 0.49),1年OS率达到20%,2年OS率达到10%,而安慰剂组均为0% 。
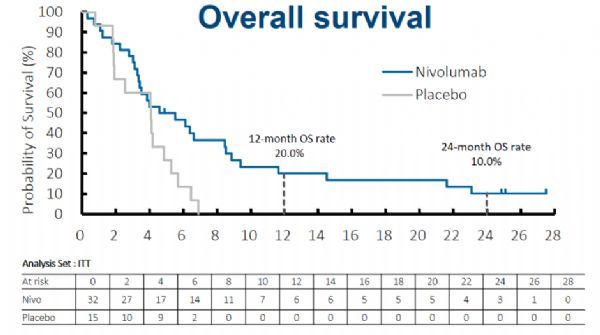
图2 ATTRACTION-2研究的中国台湾亚组OS结果
基于ATTRACTION-2研究数据,今年3月,纳武利尤单抗正式获得中国国家药品监督管理局(NMPA)批准用于治疗既往接受过两种或两种以上全身性治疗方案的晚期或复发性胃或胃食管连接部腺癌患者,成为了中国首个获批用于晚期胃癌治疗的免疫肿瘤药物,同时也是首个且迄今唯一经Ⅲ期临床研究证实能为中国晚期胃癌患者带来显著生存获益的PD-1抑制剂。
袁响林教授认为,ATTRACTION-2研究结果是一个非常重要的成果。凭借这一充分的循证证据,使纳武利尤单抗在此次指南的免疫疗法更新中脱颖而出。
一线“胃”来可期
“胃癌方向的探索性研究层出不穷,我个人是充满期待的。尽管现在还没有写进指南,但相信在不久的将来,免疫疗法用于胃癌一线治疗很可能会成为现实。“袁响林教授表示,“精准筛选患者和免疫联合治疗是目前正在探索的两大方向。”
一方面,优选人群更有望从免疫一线治疗中获益。袁响林教授提及,错配修复缺陷(dMMR)的患者人群在肠癌或其他的肿瘤治疗中,用免疫疗法都取得了比较好的疗效,对胃癌免疫治疗也具有指导意义。另外,EB病毒感染患者也可以考虑在化疗基础上加上免疫治疗。对于HER2阴性或弱阳性的其余患者,免疫疗法用于PD-L1 CPS评分较高的患者也有望走到一线。
另一方面,免疫疗法联合化疗的探索已经初具规模。纳武利尤单抗联合化疗用于胃癌一线治疗的ATTRACTION-4研究正是其中之一,根据其目前第一阶段的II期研究报道,纳武利尤单抗联合SOX方案的客观缓解率(ORR)是57.1%,联合CapeOX方案是76.5%;显著高于单纯化疗方案40%左右的结果。令人兴奋的治疗优势提升了业内对于其后续III期研究结果的期待。
无独有偶,近期胃癌及食管癌一线治疗的III期临床研究CheckMate-649初步结果亦已出炉。与单独化疗相比,纳武利尤单抗联合化疗用于PD-L1表达阳性即联合阳性评分(CPS)≥5的转移性胃癌、胃食管连接部癌或食管腺癌患者的一线治疗效果的III期临床研究达到主要研究终点总生存期(OS)和无进展生存期(PFS)。其中,本次分析OS为预先设定的中期分析, PFS为最终分析。在所有随机人群中,同样观察到OS获益。
至此,纳武利尤单抗也成为了首个且目前唯一与化疗联合用于胃癌及食管癌一线治疗获得临床研究阳性结果的免疫肿瘤药物。
相信未来,如袁响林教授所言,免疫治疗将改变胃癌治疗格局,为更多晚期胃癌患者带来生存获益。
参考文献:
[1] A phase III study of nivolumab (Nivo) in previously treated advanced gastric or gastric esophageal junction (G/GEJ) cancer (ATTRACTION-2): Three-year update data. 2020 ASCO GI, Abstract #383.
[2] Chen L-T. et al. A phase 3 study of nivolumab in previously treated advanced gastric or gastroesophageal junction cancer (ATTRACTION‑2): 2‑year update data [J]. Gastric Cancer 2019(19).
[3] Lei Y., et al. Incidence and mortality of stomach cancer in China,2014[J].Chinese Journal of Cancer Research,2018,30(03):291-298.
[4] Chao Y, Chen JS, Yeh KH, et al. Nivolumab in Advanced Gastric or Gastroesophageal Junction Cancer Refractory to, or Intolerant of, at Least Two Previous Chemotherapy Regimens: a Taiwaness Subgroup Analysis of ATTRACTION-2 Study. GEST (2019) Annual Meeting.
[5] Boku N,Ryu MH,Kato K, et al. Safety and efficacy of nivolumab in combination with S-1/capecitabine plus oxaliplatin in patients with previously untreated, unresectable, advanced, or recurrent gastric/gastroesophageal junction cancer: interim results of a randomized, phase II trial (ATTRACTION-4). Annals of Oncology 30: 250–258, 2019
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







优秀!
50
#循证#
25
赞
81
指南很好
79
!
85
!
76
!
59
精准推荐也是进一步规范临床治疗的方式之一
26