马尾肿瘤切除术
2016-03-14 MedSci www.windrug.com
马尾肿瘤切除术 马尾肿瘤可有神经鞘瘤、室管膜瘤、脊膜或先天性肿瘤(皮样囊肿、畸胎瘤等)。从手术角度看,可分为下列两种类型: 1-1 肿瘤包于马尾神经内 1-2 分离肿瘤 一种是肿瘤小而孤立,侵犯少数马尾神经,如神经鞘瘤、小的室管瘤、脊膜瘤等。这种肿瘤应充分剥离其与
马尾肿瘤切除术
马尾肿瘤可有神经鞘瘤、室管膜瘤、脊膜或先天性肿瘤(皮样囊肿、畸胎瘤等)。从手术角度看,可分为下列两种类型:
 |
 |
| 1-1 肿瘤包于马尾神经内 | 1-2 分离肿瘤 |
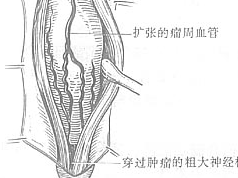
一种是肿瘤小而孤立,侵犯少数马尾神经,如神经鞘瘤、小的室管瘤、脊膜瘤等。这种肿瘤应充分剥离其与正常神经根的粘连,把肿瘤分离出来[图1-1、2]。如发生于终丝或有神经穿过肿瘤者,则可切断,提起已游离远端(也可穿线牵引)[图1-3],然后将其完整切除。这时虽同时切除个别马尾神经,但可获得根治。
 |
 |
| 1-3 提起、切断穿过肿瘤的神经,游离肿瘤 | 1-4 马尾室管膜瘤包膜内分块切除 |
另一种是较大的肿瘤把大部分马尾神经包在瘤内,如巨大的室管膜瘤[图1-4]、皮样囊肿[图1-5]等;有时慢性炎症肉芽肿也可形成同样的病变。对此种情况,如把肿瘤勉强全部切除,势必导致严重后遗症,所以只能把肿瘤包膜切开,分块切除肿瘤,与马尾神经明显粘连的部分则不作处理。术毕不缝合硬脊膜。
 |
| 1-5 马尾皮样囊肿包膜内分块切除 |
| 图1 马尾肿瘤切除术 |
[术中注意事项]
上皮样囊肿或皮样囊肿有皮肤窦道与椎管内相通者,术前或麻醉后可向窦道注入美蓝1~2ml,这样订中可沿染色区追溯到肿瘤处。
[术后处理]
同椎管-脊髓探查术。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#切除术#
27
#肿瘤切除#
29
内容精彩
95