特发性面神经麻痹的诊治,这张流程图帮您搞定
2017-03-16 李德华, 杨玲, 李季 中华神经医学杂志
特发性面神经麻痹(贝尔麻痹)是临床常见多发病,患病后患者多会立即就医,并且治愈心切,但是该病的发生、发展及预后恢复根据每位患者的具体情况不同而差别较大,临床上如何根据每位患者的具体情况治疗,国外的相关指南及处理流程值得借鉴和参考。

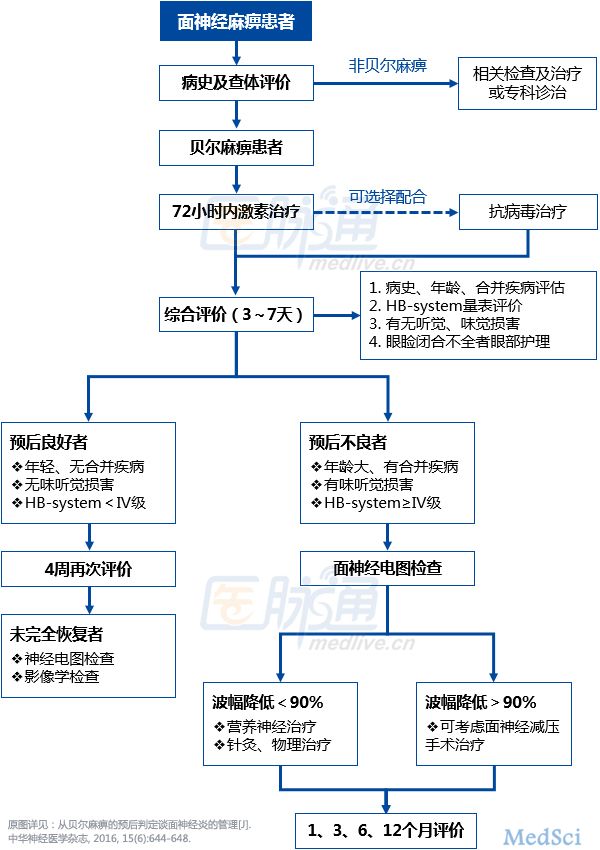
贝尔麻痹的诊治流程建议
结合国外指南建议及国内临床现状,贝尔麻痹患者诊治流程建议见下图。
关于激素和抗病毒治疗
近2年,美国神经病学会和美国耳鼻喉-头颈外科学会均发布了各自的临床指南,旨在为贝尔麻痹患者改善疾病预后和提高护理质量,国内尚无贝尔麻痹的诊断治疗指南。两版指南关于激素和抗病毒药物治疗方面做出了相同的建议,且通过不同的方式给出了建议的强度。
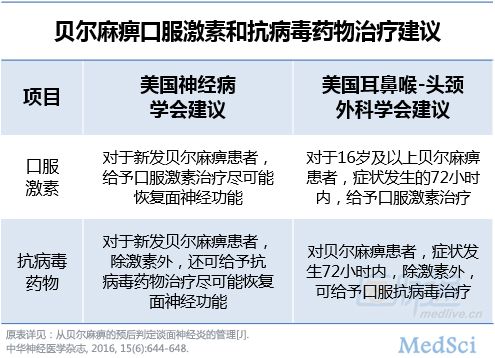
根据两个指南建议及国内现状,建议贝尔麻痹患者尽早足量使用激素治疗,强的松使用剂量可以参考每天1 mg/kg,连用7天后逐天减量。关于抗病毒药物的使用,系统评价显示对于贝尔麻痹患者单用抗病毒药物患者并不能获益,抗病毒药物结合激素一起使用有可能提高患者完全恢复的比率,指南建议根据患者评估情况,症状较重预后不良的新发病患者72小时内抗病毒联合激素一起使用。
抗病毒常用药物有阿昔洛韦或伐昔洛韦,阿昔洛韦用量为5~10 mg/kg,3次/天,连用7天;伐昔洛韦成人500 mg,3次/天,连用7天。
关于针灸及其它治疗
针灸治疗面神经麻痹在我国临床广泛使用并有大量的临床报道,但是由于文献质量不高,系统评价关于针刺治疗面神经有效性和安全性得不到充分的证据支持,所以该疗法在两个指南中都未做推荐使用,但是同时也提出希望有严格设计的高质量的随机对照试验证据来支持这种疗法,美国神经病学会指南中指出在恢复阶段的患者可以使用针灸治疗。
在国内,针灸疗法做为面瘫的一种主要治疗方法,患者信赖并取得了一定的临床疗效,因此有必要遵循临床流行病学、循证医学设计原则来客观评价,使这一传统疗法让更多人受益。
高压氧治疗虽有报道对面神经麻痹有益,但也由于缺乏高质量的证据使得系统评价得不到有力支持,在指南中都未做推荐使用。其他如电刺激治疗、煅炼、光、波等物理治皆因临床证据不足在指南未做推荐使用。
小结
由于每位患者的个体情况不同,面瘫的预后又受诸多因素影响,因此对于每位患者都有必要进行评估并进行及时有效的治疗,对于新发病患者应早期使用激素及根据患者症状联合使用抗病毒药物治疗,在恢复阶段可根据个体情况配合使用针灸、高压氧、物理治疗等手段,以促使患者尽可能最大功能恢复,同时又避免对于轻度可自愈的患者过度治疗。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#面神经#
41
#特发性#
0
感谢分享,学习最新进展
1
认真学习,谢谢分享
36
要求认真学习和鉴别
40
学习了谢谢了。
42
#面神经麻痹#
28