日前,美国耶鲁大学(Yale University)的研究团队发现一个在低密度脂蛋白(LDL) 胆固醇在血管内沉积过程中起到重要作用的蛋白,这为阻断LDL沉积的创新医疗方法的开发提供了启示,从而防止或者减缓导致心脏疾病的血管阻塞。这项研究成果发表在《自然》子刊Nature Communications上。
动脉粥样硬化导致的心血管疾病是世界范围内第一大致死因素。动脉粥样硬化的产生是因为脂蛋白,尤其是LDL,与血液中的脂肪和胆固醇相结合,并且将它们运输穿过构成血管内壁的内皮细胞,而脂肪和胆固醇在内皮下区域的沉积是导致动脉粥样硬化的重要原因。
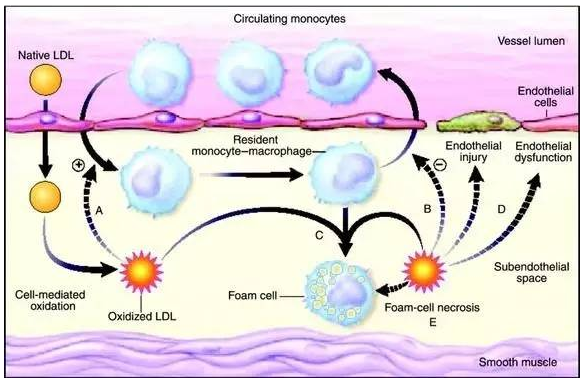
▲LDL引发动脉粥样硬化(图片来源:particulatefouling)
目前,防止这类疾病最有效的疗法是降低血液中LDL的水平,这样可以减少LDL脂蛋白颗粒进入并且驻留在血管壁中的可能性。然而,LDL如何被运输穿过血管内皮的分子机制一直没有完全得到阐明。长期以来,科学家们认为LDL受体担负着在细胞内运输LDL的功能。不过,一些体内没有LDL受体的人仍然会产生高水平的LDL沉积,这其中发生机制仍然是一个未解之谜。
为了找到LDL运输的机制,耶鲁大学的研究人员运用RNAi库对1万8千多个基因进行了筛选。他们把研究重点放在那些影响LDL向内皮细胞内运输的基因上上。研究结果表明,一种称为ALK1的蛋白能够帮助LDL向细胞内的转移。ALK1能够直接与LDL相结合,并且通过一个特别的内吞通路 (Endocytic Pathway) 促进LDL穿过内皮细胞进入内皮下组织,而不是将LDL导入溶酶体降解。如果在小鼠的内皮组织中特异性地敲除ALK1基因,则会导致血管内皮摄入的LDL水平下降。

▲文章的通讯作者William C. Sessa教授(图片来源:Yale)
“发现ALK1蛋白能够与LDL结合,意味着它可能引发早期动脉粥样硬化,”文章的通讯作者、耶鲁大学教授William C. Sessa说:“如果我们发现能够阻断ALK1蛋白的小分子或者抗体,则可能与其它降血脂疗法联合使用,来降低动脉粥样硬化的风险。”
原始出处:
[1] Jan R. Kraehling, William C. Sessa,et al. Genome-wide RNAi screen reveals ALK1 mediates LDL uptake and transcytosis in endothelial cells. Nature Communications.21 November 2016.
[2] Study finds key protein that binds to LDL cholesterol. Medical Press.November 21, 2016.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#粥样硬化#
29
#Nat#
24
#新靶点#
29
继续关注
46
期待得到更多的这方面消息!有趣
46
alk-1蛋白与ldl结合途径是低密度脂蛋白进入细胞导致动脉粥样硬化的方式之一(或是主要方式),这应该不是唯一途径,应该还有别的途径。但,这个途径的作用是什么?它对人体的意义是什么?
42
alk1.ldl.血脂沉积,动脉粥样硬化,冠心病
56
期待进一步的研究成果
42
期待新药的开发研究
22
谢谢分享!
23