Sicot J:一例典型的运动过量出现的股骨颈应力性骨折
2019-04-24 林嘉琛 医博士
患者女,27岁,诉长跑训练后左侧腹股沟疼痛。长跑训练强度高,要求30分钟内完成6km,并着军装军靴和4.5kg重的来复枪。在口服双氯芬酸钠一周后疼痛仅有部分缓解,于是要求军医提供肌内注射镇痛治疗。
患者女,27岁,诉长跑训练后左侧腹股沟疼痛。长跑训练强度高,要求30分钟内完成6km,并着军装军靴和4.5kg重的来复枪。在口服双氯芬酸钠一周后疼痛仅有部分缓解,于是要求军医提供肌内注射镇痛治疗。
三周后患者自觉症状加重。体检无畸形可见,左侧髋关节主被动运动范围减少,伴疼痛。患肢灌注状态正常。X平片未见骨折或急性损伤(图1),但上述症状依然持续了2周,休息无缓解,因此继续进行了CT扫描,发现左侧股骨颈骨皮质组织结构紊乱(图2)。MRI提示左侧股骨颈FNFS不伴脱位(图3)。骨折线大约包绕了一半左右的股骨颈全长。

图1

图2
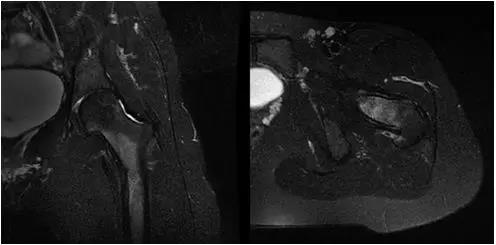
图3
给予患者无负重6周休息的医嘱,随后进行部分负重的活动。患者于3个月开始正常的日常活动。6个月后症状消失。随访可见骨折线愈合良好,无延迟愈合或缺血性坏死等表现(图4)。患者于18个月后重返正常军队训练。
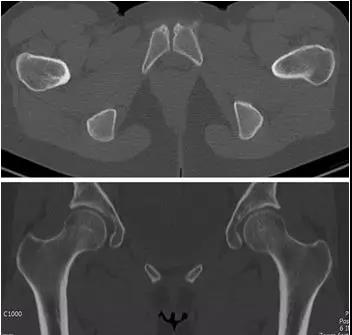
图4
讨论及小结
应力性骨折的定义是长期或者反复的机械应力引起的骨结构性损伤,可分为疲劳性(负重过载)和病理性(骨质下降)。对于军人,FNSF是具有生涯毁灭性的,因为FNFS位置的特殊性导致回复周期很长。FNFS的临床表现通常包括腹股沟疼痛、不能负重、压痛等等,体检可见跛行和运动范围受限。
原始出处:
Hélder Fonte, Rodrigues-Pinto R . Femoral neck stress fracture in a young female recruit: case report[J]. Sicot J, 2018.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#SICOT#
26
#股骨颈#
25
#股骨#
32
#应力#
39