TC-210治疗难治性间皮素阳性实体瘤:I/II期临床试验取得积极结果
2020-12-16 Allan MedSci原创
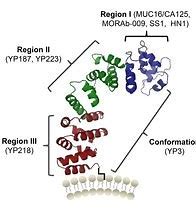
间皮素(MSLN)是多种肿瘤表面特异性表达的受体蛋白,特别是在以胰腺癌(80%~85%)为首的多种实体肿瘤中高表达,而在正常组织中间皮素的表达仅局限于胸膜、心包膜和腹膜中。
间皮素(MSLN)是多种肿瘤表面特异性表达的受体蛋白,特别是在以胰腺癌(80%~85%)为首的多种实体肿瘤中高表达,而在正常组织中间皮素的表达仅局限于胸膜、心包膜和腹膜中。
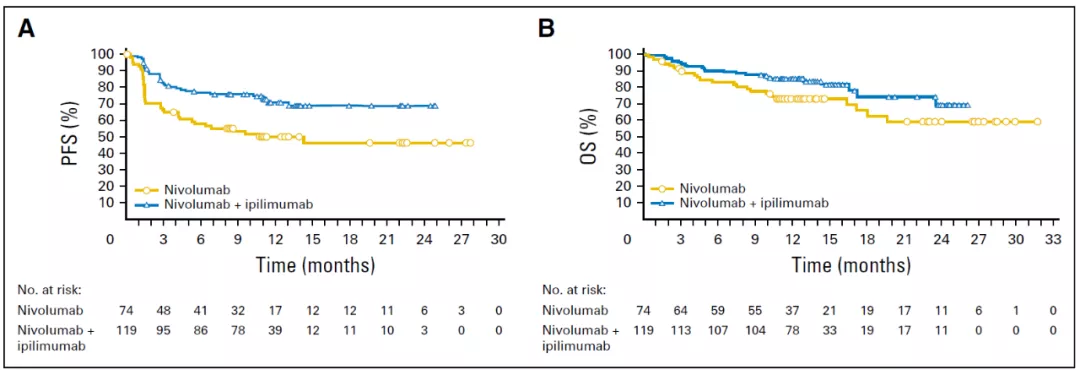
TCR²是一家临床阶段的免疫疗法公司,今天宣布了来自TC-210(gavocabtagene autoleucel)治疗间皮素阳性实体瘤的I/II期临床试验结果。截至2020年11月24日的数据截止,在前8名患者中已记录了根据RECIST 1.1标准的3例PR,而首例卵巢癌患者在第6个月已取得PR。迄今为止,只有2名患者出现了与gavocabtagene autoleucel相关的非血液学分级毒性,并且没有神经毒性及非肿瘤毒性的证据。
TCR² Therapeutics总裁兼首席执行官Garry Menzel博士说:“尽管任何一项I期临床试验的重点都是安全性,但我们使用gavocabtagene autoleucel作为单一药物观察到的肿瘤消退支持了我们对TRuC-T细胞的信念。最重要的是,我们正在为那些经过高度预处理的间皮瘤或卵巢癌患者提供临床和生存益处”。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#I期临床试验#
45
#II期临床试验#
42
#I期临床#
33
#II期临床#
29
#难治性#
37
学习了
84