Hypertension:血管生成抑制诱导血压升高的盐敏感性!
2017-03-21 xing.T MedSci原创
由此可见,舒尼替尼可以诱导高血压,可以被摄入高盐而加重,但不伴有皮肤淋巴管受损。
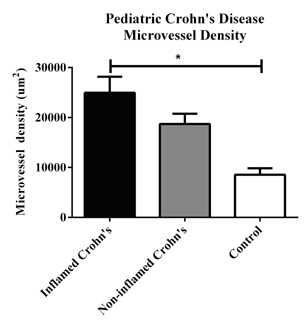
为响应盐负荷,皮肤中Na+和Cl-聚集和过量水分,刺激皮肤淋巴管生成通过激活单核吞噬细胞系统来源的血管内皮生长因子-C-血管内皮生长因子3型受体信号转导通路。该通路的抑制可以导致盐敏感性高血压。舒尼替尼是一种抗血管生成、抗癌剂,可以阻断所有血管内皮生长因子3型受体并且升高血压。近日,心血管权威杂志Hypertension上发表了一篇研究文章,研究人员探讨了舒尼替尼诱导高血压的盐依赖性,并且评估了皮肤淋巴管生成障碍是否是其发生的一个潜在的机制。
研究人员将血压正常的Wistar–京都大鼠暴露于正常或高盐,并给予或不给予舒尼替尼处理。通过遥感测量发现舒尼替尼诱导血压上升15mmHg,并且这可以被高盐饮食(HSD)所加重,导致压力-钠曲线的斜率下降。并不影响体重、血浆钠离子浓度或肾功能、在高盐组大鼠Na+和Cl-的皮肤含量分别增加了31%和32%,而在HSD联合舒尼替尼组分别增加了49%和50%,而皮肤水含量分别增加了17%和24%。皮肤单核吞噬细胞系统的细胞密度在接触舒尼替尼和HSD期间都有所增加,当将HSD和舒尼替尼联合时,但没有观察到进一步的增加。HSD增加皮肤淋巴管生成,而舒尼替尼趋于减少淋巴管生成,在正常盐饮食和HSD。
由此可见,舒尼替尼可以诱导高血压,可以被摄入高盐而加重,但不伴有皮肤淋巴管受损。
原始出处:
Stephanie Lankhorst, et al. Salt Sensitivity of Angiogenesis Inhibition–Induced Blood Pressure Rise Role of Interstitial Sodium Accumulation?.Hypertension. 2017. https://doi.org/10.1161/HYPERTENSIONAHA.116.08565
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
32
#TENS#
24
#血压升高#
29
#盐敏感#
28
#敏感性#
25
#Hypertension#
27