Diabetologia:早期红色病变的空间分布是发展成糖尿病视网膜病视力损伤的危险因素
2017-12-31 MedSci MedSci原创
研究发现进展为视力损伤的糖尿病性视网膜病变的可能性在黄斑中心的圆形区域中更高,并且该区域中的第一个病变的发生预示着视力损伤的糖尿病视网膜病变的发展。计算的峰值显示进展的风险比平均值高39.5%。在迟发糖尿病黄斑病变或增生性糖尿病性视网膜病变的病人损伤早期分布没有显著差异。
近日,国际杂志 《Diabetologia》上在线发表一项关于早期红色病变的空间分布是发展成糖尿病视网膜病视力损伤的危险因素的研究。
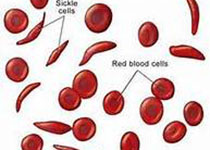
糖尿病视网膜病的特征是出现与视网膜血流紊乱有关的形态学损害。先前研究已经表明,视网膜中央凹病变的早期发展可以预测需要治疗的糖尿病黄斑病变的发展。这项研究的目的是准确地定位损伤位点,进而可以预测视网膜病变的进展。
在观察期间通过比较晚期视力损伤的糖尿病视网膜病变的个体与之糖尿病类型,年龄,性别和发病年龄相匹配的没有发展成视力受损糖尿病性视网膜病的个体,研究代表出血和/或微动脉瘤的最早红色病变位置的预测价值。
研究发现进展为视力损伤的糖尿病性视网膜病变的可能性在黄斑中心的圆形区域中更高,并且该区域中的第一个病变的发生预示着视力损伤的糖尿病视网膜病变的发展。计算的峰值显示进展的风险比平均值高39.5%。在迟发糖尿病黄斑病变或增生性糖尿病性视网膜病变的病人损伤早期分布没有显著差异。
研究表明,早期红色病变在糖尿病性视网膜病变中的位置预示着个体是否会后来发展为视力损伤糖尿病视网膜病变。这个证据应该被纳入用于推荐糖尿病视网膜病筛查项目控制的风险模型。
原始出处:
Giovanni Ometto, Phil Assheton, Francesco Calivá,et al. Spatial
distribution of early red lesions is a risk factor for development of
vision-threatening diabetic retinopathy
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#DIA#
18
#BET#
22
#空间分布#
34
#视网膜#
29
#损伤#
28
非常好.谢谢分享
43
厉害了我的哥
44