ISC2018:医学卒中急救奖获得者介绍运筹学和数据科学在心血管病中的应用
2018-01-27 国际循环编辑部 国际循环
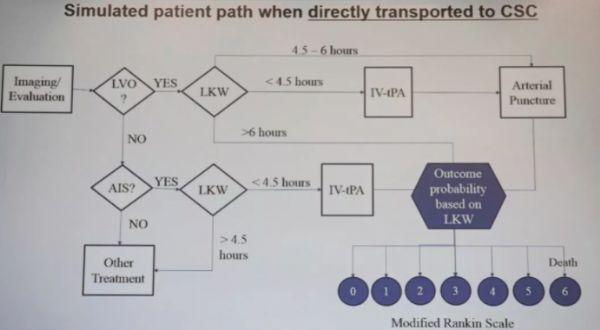
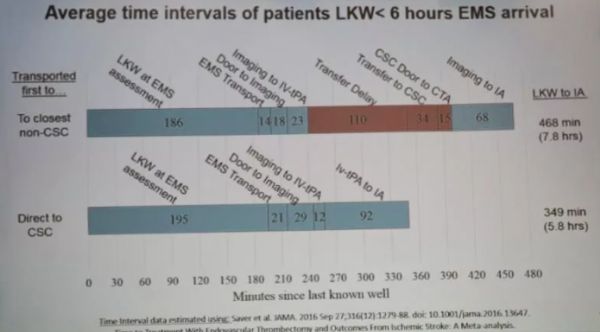
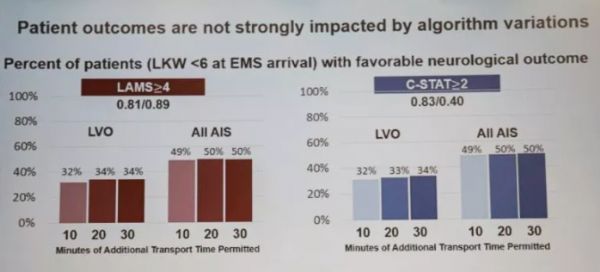
美国北卡罗莱纳大学荣获ISC 2018医学卒中急救奖在会上发表题为“采用离散事件仿真评估基于严重程度的EMS卒中分类转运流程对患者结局及分流的区域特异性影响”的精彩演讲,并接受了采访。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#数据科学#
35
#卒中急救#
30
#血管病#
30
#ISC#
28
^_^^_^^_^^_^^_^
59
阅
55