JACC:可预测Fontan术后死亡或心脏移植风险的临床和CMR指标
2021-05-24 Nebula MedSci原创
对于Fontan手术后的患者,心室扩张增加是死亡或心脏移植的最强独立预测指标
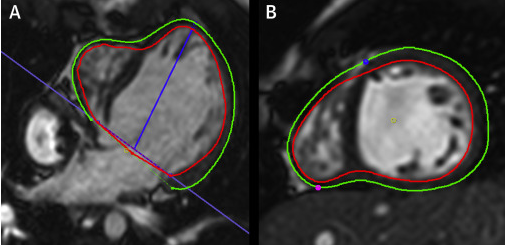
Fontan手术又称“肺动脉下心室旷置术”,是治疗三尖瓣闭锁、单心室、肺动脉闭锁、多脾症、无脾症等复杂心内畸形的惟一的心内矫治方法。某些临床和心脏磁共振(CMR)参数已显示出在与Fontan手术后的死亡或晚期心脏移植风险相关。

本研究旨在明确Fontan手术后的临床和CMR参数对于分层风险的相对重要性和相互影响。
对进行了Fontan手术的患者进行回归性分析。采用单变量Cox回归分析临床和CMR参数。主要终点是死亡或心脏移植(进入心脏移植名单)的时间。
共纳入了46位患者,男性占62%,中位年龄为16岁(25%-75%:11-23岁)。CMR后的中位随访时间为5.4年(25%-75%:2.4-10.0,57位患者(14%)达到了终点(46例死亡、7例心脏移植、4例列入心脏移植名单)。
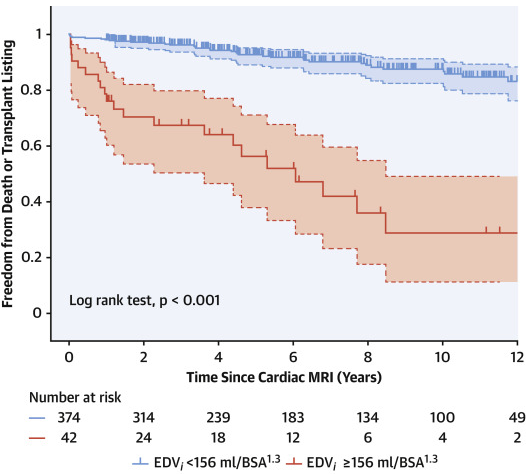
高EDVi和低EDVi患者的死亡或心脏移植风险
较低的总舒张末期容积指数(EDVi)是无移植生存期的最强预测指标。在EDVi较高(EDVi≥156ml/BSA1.3)的患者中,较差的整体圆周应变(GCS)是第二重要的预测指标(73% vs 44%)。在EDVi较低(EDVi<156ml/BSA1.3)的患者中,纽约心脏协会功能分类(NYHA)II级及以上是次要的预测指标(30% vs 4%)。
根据舒张末期容积、他汀和NYHA分类的预后
综上,对于Fontan手术后的患者,心室扩张增加是死亡或心脏移植的最强独立预测指标。伴有心室扩张和GCS恶化的患者的风险最高。这些数据凸显了将CMR和临床参数相结合用于该人群风险分层的价值
原始出处:
Meyer Sophie L,St Clair Nicole,Powell Andrew J et al. Integrated Clinical and Magnetic Resonance Imaging Assessments Late After Fontan Operation. J Am Coll Cardiol, 2021, 77: 2480-2489. https://doi.org/10.1016/j.jacc.2021.03.312
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CMR#
43
#JACC#
0
#Fontan#
48
#ACC#
32