EUR J Cancer:转移性结直肠癌患者经化疗联合西妥昔单抗或贝伐单抗治疗后的手术可行性评估:FIRE-3临床试验评估
2017-12-24 MedSci MedSci原创
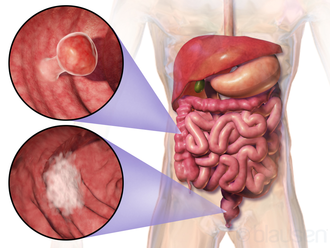
FIRE-3临床试验研究了化疗联合西妥昔单抗或贝伐单抗治疗未经治疗的转移性结直肠癌(mCRC),德国慕尼黑大学的研究人员通过该临床试验,确定了经系统性一线治疗方案后具有潜在肿瘤可切除性的mCRC患者数量,并将这些研究结果和那些关注可切除性的研究作了详细对比。研究人员对448名患者的治疗结果进行了盲法评估,而可切除性的定义是否至少有50%的评价者推荐手术干预,总生存期则用Kaplane-Meier法
FIRE-3临床试验研究了化疗联合西妥昔单抗或贝伐单抗治疗未经治疗的转移性结直肠癌(mCRC),德国慕尼黑大学的研究人员通过该临床试验,确定了经系统性一线治疗方案后具有潜在肿瘤可切除性的mCRC患者数量,并将这些研究结果和那些关注可切除性的研究作了详细对比。
研究人员对448名患者的治疗结果进行了盲法评估,而可切除性的定义是否至少有50%的评价者推荐手术干预,总生存期则用Kaplane-Meier法进行评估。
结果显示,经化疗联合西妥昔单抗或贝伐单抗治疗后,肿瘤的可切除性从治疗前的22%(97/448)增加到了53%(238 /448)(P <0.001)。总生存期在接受手术的可切除病人中为51.3个月(95%置信区间35.9-66.7);在未接受手术的可切除病人中为30.8个月(95%置信区间26.6-34.9);在不能切除的患者中为18.6个月(95%置信区间15.8-21.3)(P <0.001)。
因此,该项研究阐明了经化疗联合西妥昔单抗或贝伐单抗治疗后手术切除性的可能,对提高转移性结直肠癌患者总生存期具有重要意义。
原始出处:
Modest, Dominik P.,
et al. "Surgical treatment options following chemotherapy plus cetuximab
or bevacizumab in metastatic colorectal cancer—central evaluation of
FIRE-3." European Journal of Cancer 2018 88: 77-86. doi.org/10.1016/j.ejca.
本文系梅斯医学(MedSci)原创编译整理,转载需授权
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#FIRE-3#
31
#西妥昔#
37
#可行性#
29
#转移性#
22
#结直肠#
33
#贝伐#
32