NEJM:巴龙霉素单药或合并庆大霉素治疗皮肤利什曼病效果显著
2013-05-16 NEJM dxy
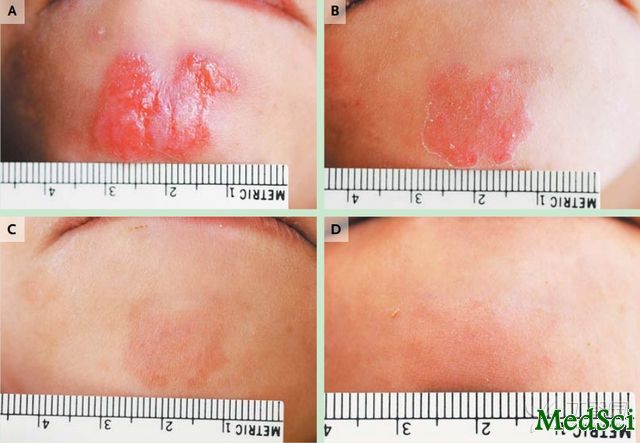
治疗中典型损伤的反应 医学界迫切需要找到一种简单、有效且其副作用能够被接受的方法来治疗皮肤利什曼病。突尼斯突尼斯市巴斯德研究所Afif Ben Salah博士等人的研究显示,巴龙霉素-庆大霉素联合应用以及巴龙霉素单独用药治疗溃疡性硕大利什曼原虫疾病均安全有效。相关论文近期发表于国际权威杂志NEJM在线版上。研究人员在突尼斯进行了一项随机对照的3期试验,对局部15%巴龙霉素单一使用或与0.5%庆大
医学界迫切需要找到一种简单、有效且其副作用能够被接受的方法来治疗皮肤利什曼病。突尼斯突尼斯市巴斯德研究所Afif Ben Salah博士等人的研究显示,巴龙霉素-庆大霉素联合应用以及巴龙霉素单独用药治疗溃疡性硕大利什曼原虫疾病均安全有效。相关论文近期发表于国际权威杂志NEJM在线版上。
研究人员在突尼斯进行了一项随机对照的3期试验,对局部15%巴龙霉素单一使用或与0.5%庆大霉素联合应用治疗硕大利什曼原虫导致的皮肤利什曼病方案进行研究。研究者将375例患有1~5处皮肤利什曼病溃疡性病变的患者随机分配,分别接受15%巴龙霉素-0.5%庆大霉素软膏(称为WR 279396)、或15%巴龙霉素软膏、或对照(与其他两种软膏的基质相同,但是不含巴龙霉素或庆大霉素)治疗。每处皮肤病变均治疗20天,1次/天。试验主要终点为标准损伤(index lesion)的治愈率。治愈定义为试验42天时病变损伤面积至少缩小50%,98天时完成表皮细胞再生,以及试验结束时(168天时)无复发。试验中的任何中止用药均视为治疗失败。
结果显示,巴龙霉素-庆大霉素组的标准损伤治愈率为81%[95%可信区间(CI)73~87],单用巴龙霉素组为82%(95%CI为74~87),对照治疗为58%(95%CI为50~67)(每个治疗组与对照组相比,P值均<0.001)。除5例患者外(两个治疗组各1例,以及对照组3例),其他患者在治愈标准损伤的同时,其他损伤也均治愈。轻度至中度用药部位反应在两个用药组中更常见。
研究者由此得出结论,这项试验为巴龙霉素-庆大霉素联合应用以及巴龙霉素单独用药治疗溃疡性硕大利什曼原虫疾病的有效性提供了证据。

Topical Paromomycin with or without Gentamicin for Cutaneous Leishmaniasis
Background
There is a need for a simple and efficacious treatment for cutaneous leishmaniasis with an acceptable side-effect profile.
Methods
We conducted a randomized, vehicle-controlled phase 3 trial of topical treatments containing 15% paromomycin, with and without 0.5% gentamicin, for cutaneous leishmaniasis caused by Leishmania major in Tunisia. We randomly assigned 375 patients with one to five ulcerative lesions from cutaneous leishmaniasis to receive a cream containing 15% paromomycin–0.5% gentamicin (called WR 279,396), 15% paromomycin alone, or vehicle control (with the same base as the other two creams but containing neither paromomycin nor gentamicin). Each lesion was treated once daily for 20 days. The primary end point was the cure of the index lesion. Cure was defined as at least 50% reduction in the size of the index lesion by 42 days, complete reepithelialization by 98 days, and absence of relapse by the end of the trial (168 days). Any withdrawal from the trial was considered a treatment failure.
Results
The rate of cure of the index lesion was 81% (95% confidence interval [CI], 73 to 87) for paromomycin–gentamicin, 82% (95% CI, 74 to 87) for paromomycin alone, and 58% (95% CI, 50 to 67) for vehicle control (P<0.001 for each treatment group vs. the vehicle-control group). Cure of the index lesion was accompanied by cure of all other lesions except in five patients, one in each of the paromomycin groups and three in the vehicle-control group. Mild-to-moderate application-site reactions were more frequent in the paromomycin groups than in the vehicle-control group.
Conclusions
This trial provides evidence of the efficacy of paromomycin–gentamicin and paromomycin alone for ulcerative L. major disease. (Funded by the Department of the Army; ClinicalTrials.gov number, NCT00606580.)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#利什曼病#
38
#庆大霉素#
30
不错不错!
107