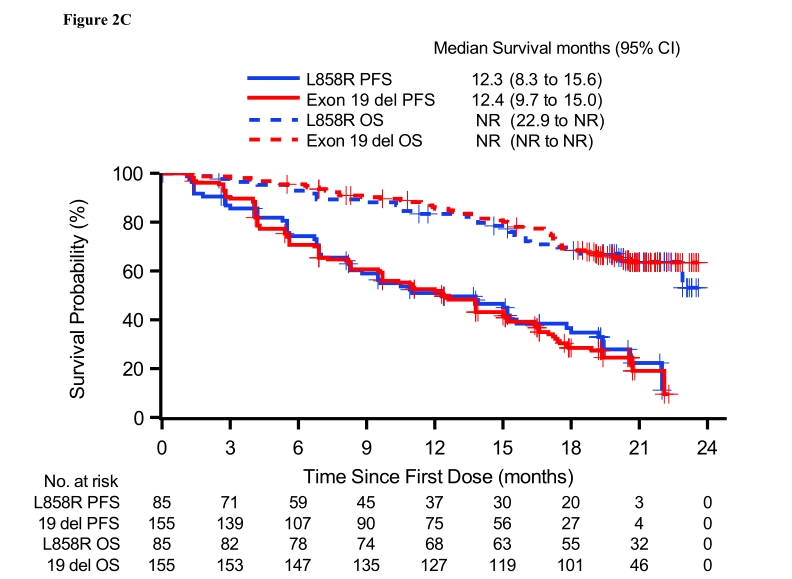
J Thorac Oncol:Aumolertinib(HS-10296)治疗EGFR-T790M+晚期NSCLC患者的疗效和安全性:APOLLO研究
2021-11-27 yd2015 MedSci原创
Aumolertinib(原almonertinib;HS-10296)是一种新型的、不可逆的第三代EGFR TKI,由Hansoh Pharmaceutical Group Co. (Shangha
Aumolertinib(原almonertinib;HS-10296)是一种新型的、不可逆的第三代EGFR TKI,由Hansoh Pharmaceutical Group Co. (Shanghai, China)开发,可选择性同时抑制EGFR敏感和T790M突变。之前I期研究 (NCT0298110)确定推荐剂量为110mg/日。中国进行的APOLLO (NCT02981108) 研究则进一步评估aumolertinib治疗T790M+晚期NSCLC患者的疗效和安全性。近期,相关结果发表在Journal of Thoracic Oncology杂志上。
研究主要纳入局部晚期或转移性NSCLC患者经过第一代或第二代EGFR-TKI治疗进展并伴有T790M突变。纳入患者服用aumolertinib 110mg/次/日。主要研究终点为独立评估委员会(ICR)评估的ORR。
研究纳入244例EGFR-T790M+ NSCLC患者。中位随访时间为19.4个月(IQR: 13.3-20.8)。中位暴露持续时间为14.2个月(IQR: 6.9-20.6;范围:0.2 - -23.6)。共有74名患者在数据截止时仍在服用aumolertinib。
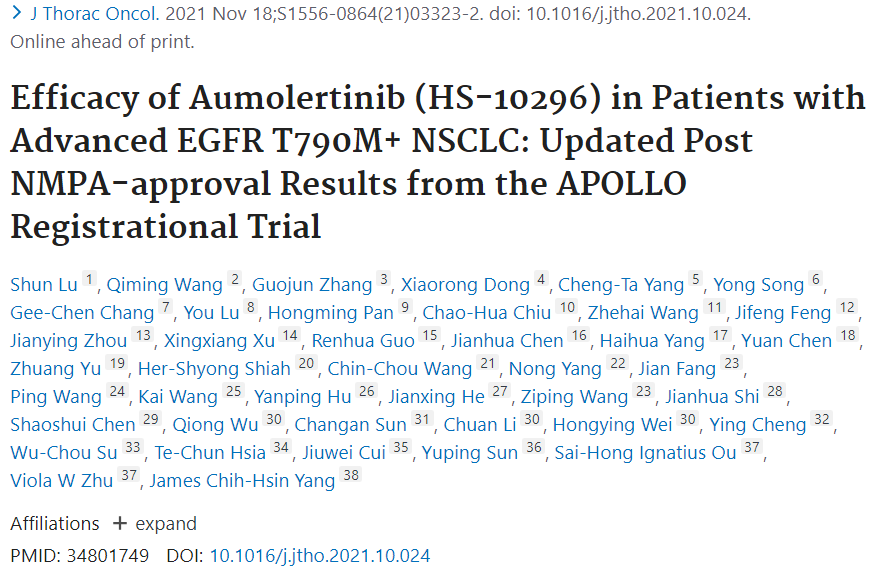
ICR证实的ORR和DCR为68.9% (168/244;95% CI: 62.6%-74.6%)和93.4% (228/244;95% CI: 89.6%-96.2%)。从基线变化的平均最佳百分比为-52.0% (95% CI: -49.0%至-55.0%)。EGFR外显子19缺失和L858R突变患者的ORR分别为72.2% (95% CI: 64.5% -79.1%)和63.5% (95% CI: 52.4% -73.7%)。共有30例患者在使用一线EGFR抑制剂后接受化疗,ORR为76.7% (95% CI: 57.7%-90.1%)。
疗效评估
中位DOR为15.1个月(95% CI: 12.5-16.6);EGFR外显子19缺失和L858R突变患者的DOR分别为15.1个月 (95% CI: 12.5-16.1) 和16.5个月 (95% CI: 10.9-19.3)。接受aumolertinib作为二线或三线治疗时DOR分别为15.8个月(95% CI: 13.8-17.8) 和12.5个月 (95% CI: 7.0-16.1)。6、9和12个月应答率分别为82.5% (95% CI: 75.9%-87.5%), 69.5% (95% CI: 61.8%-76.0%) 和62.3% (95% CI: 54.4%-69.3%)。

DOR
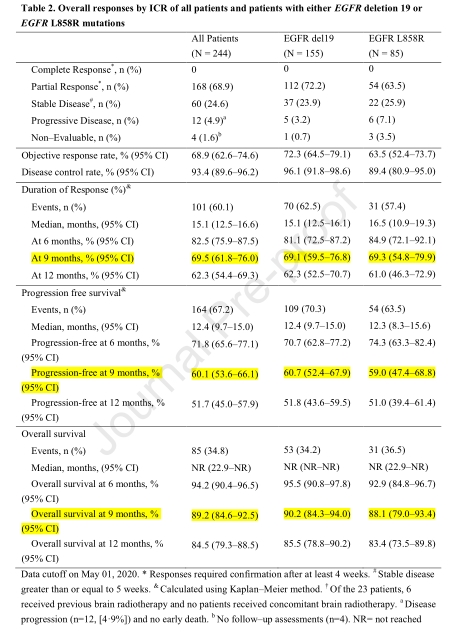
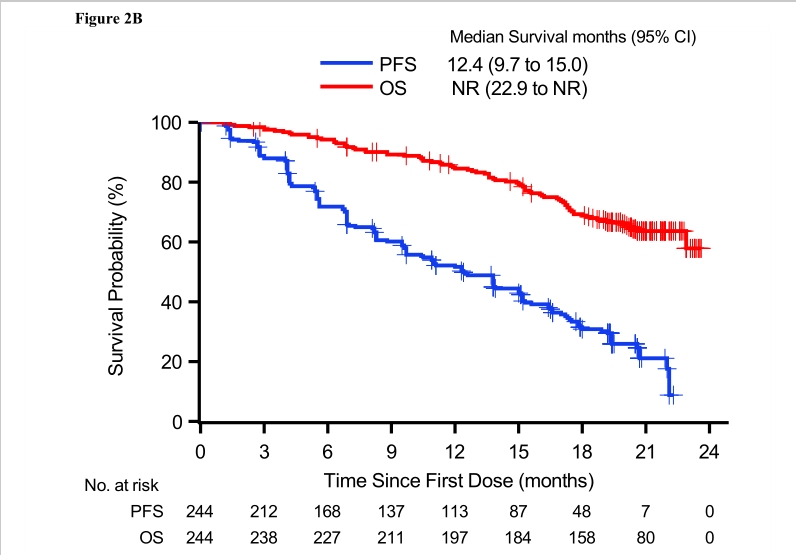
244例患者的中位PFS为12.4个月(95% CI: 9.7-15.0)。EGFR外显子19缺失和L858R突变患者的中位PFS分别为12.4个月(95% CI: 9.7-15.0)和12.3个月(95% CI: 8.3-15.6)。局部进展和转移性患者的中位PFS分别为17.0个月(95% 8.3-19.4)和12.0个月(95% CI: 9.6-13.8)。转移性患者二线接受aumolertinib治疗时,EGFR外显子19缺失和L858R突变患者的中位PFS分别为12.3 个月(95% CI: 8.3-15.1) and 10.9个月(95% CI: 7.0-17.8)。6、9和12个月PFS率分别为71.8% (95% CI: 65.6%-77.1%), 60.1% (95% CI: 53.6%-66.1%) 和51.7% (95% CI: 45.0%-57.9%)。
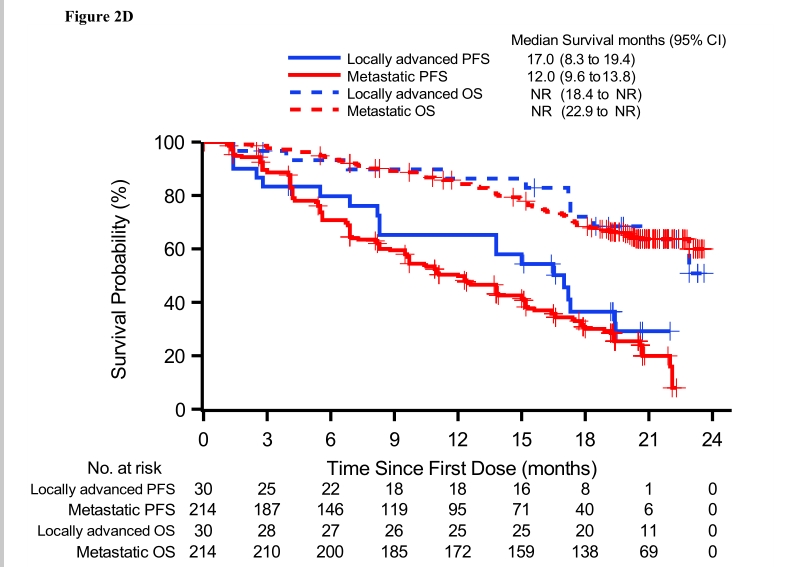
PFS和OS以及亚组分析
所有患者的中位OS为NR (95% CI: 22.9-NR)。EGFR 外显子19缺失或EGFR L858R突变患者的中位OS分别为NR (95% CI: 394 NR-NR)和NR (95% CI: 22.9-NR)。局部晚期和转移性患者的中位OS分别为NR (95% CI: 18.4-NR)和NR (95% CI: 22.9-NR)。OS率分别为:6个月94.2% (95% CI: 90.4%-96.5%)、9个月89.2% (95% CI: 84.6%-92.5%)、12个月84.5% (95% CI: 79.3%-88.5%)和18个月68.8% (95% CI: 62.5%-74.4%)。
23例伴有可测量脑转移患者中,ICR评估的ORR和DCR分别为60.9% (95% CI: 38.5-80.3) 和91.3% (95% CI: 72.0-98.9)。DOR为12.5个月(95% CI: 5.6-NR)。中位PFS为11.8个月(95% CI: 5.5-15.3)。中位OS位16.2个月(95% CI: 11.8-20.4)。
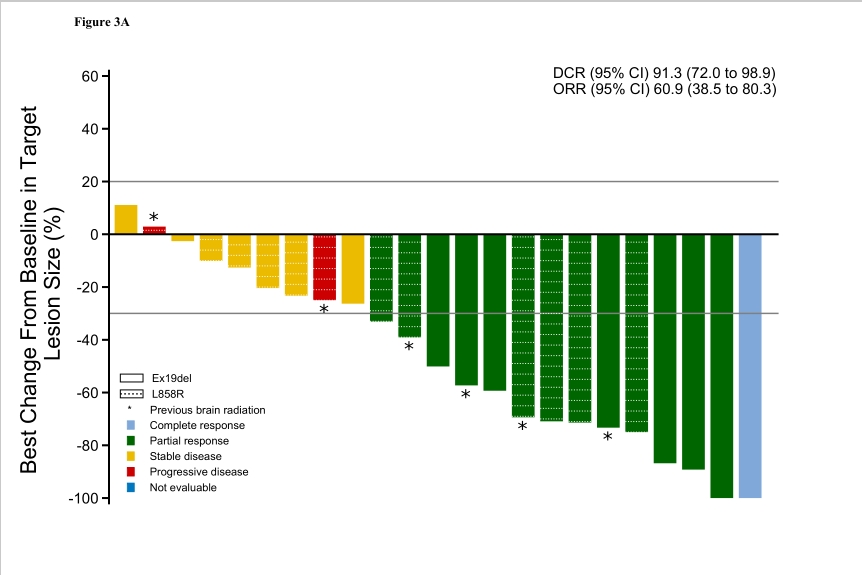
颅内应答
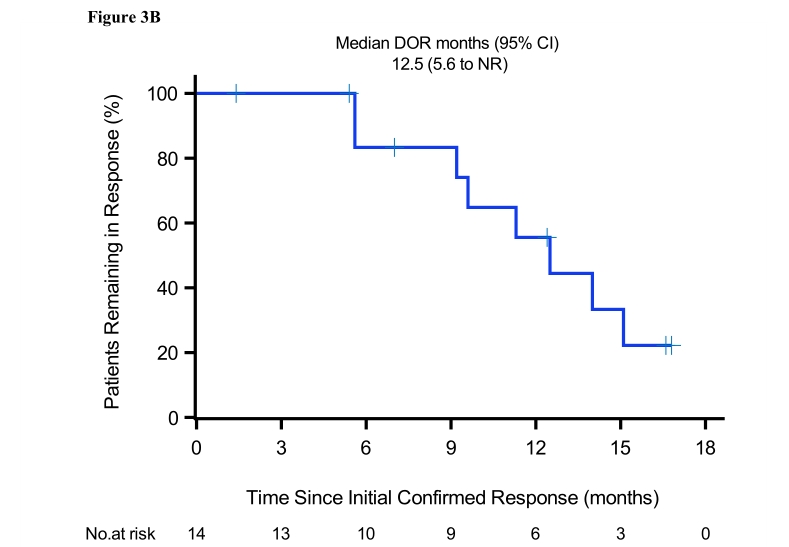
颅内DOR
16.4%的患者发生≥3级治疗相关不良事件,最常见的是血肌酸磷酸激酶升高(7%)和丙氨酸转氨酶升高(1.2%)。
综上,研究表明,第三代EGFR-TKI aumolertinib治疗EGFR-T790M突变NSCLC患者疗效显著并且耐受性良好。
Lu S, Wang Q, Zhang G, et al. Efficacy of Aumolertinib (HS-10296) in Patients with Advanced EGFR T790M+ NSCLC: Updated Post NMPA-approval Results from the APOLLO Registrational Trial. J Thorac Oncol. 2021 Nov 18:S1556-0864(21)03323-2. doi: 10.1016/j.jtho.2021.10.024. Epub ahead of print. PMID: 34801749.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#SCLC患者#
38
#疗效和安全性#
32
#Oncol#
36
#T790M#
32
#THORAC#
27
#NSCLC患者#
33
#晚期NSCLC#
39
#S-1#
35
#GFR#
25