Geburtshilfe Frauenheilkd:导管原位癌的预后评价
2014-12-25 MedSci MedSci原创
Geburtshilfe Frauenheilkd:导管原位癌的预后评价 研究背景:由于乳腺癌筛查手段的进步,更多的导管原位癌(DCIS)被早期发现,并非所有的DCIS未经治疗都会进展为浸润性乳腺癌(IBC),但是一旦发现DCIS大部分多会治疗,但是目前缺少DCIS的危险分层,以便个性化治疗,减少不必要的治疗。 研究目的:对DCIS进行危险分层,以便指导其治疗及提供预
研究背景:
由于乳腺癌筛查手段的进步,更多的导管原位癌(DCIS)被早期发现,并非所有的DCIS未经治疗都会进展为浸润性乳腺癌(IBC),但是一旦发现DCIS大部分多会治疗,但是目前缺少DCIS的危险分层,以便个性化治疗,减少不必要的治疗。
研究目的:
对DCIS进行危险分层,以便指导其治疗及提供预后信息。
研究方法:
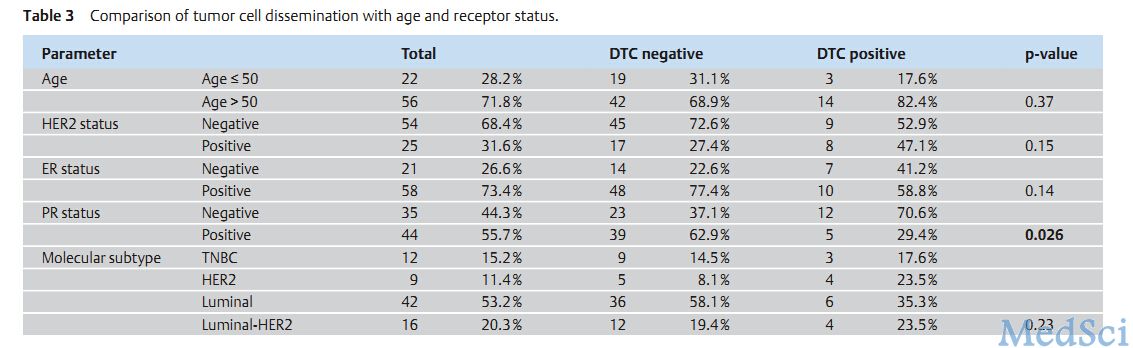
纳入2004年1月-2011年11月德国法兰克福市歌德医院乳腺科145名IBC和DCIS患者(53DCIS、92IBC),随后又增加了24名DCIS和31名T1aIBC患者;另外纳入60名(61IBC、29DCIS)患者检查其弥散肿瘤细胞(DTC)。回顾其病理检查及免疫组化检查结果,并将所有患者分为4种亚型TNBC、HER2(ER-/HER2+)、luminal(ER+/HER2-)、luminalHER2(ER+/HER2+),运用SPSS进行统计学分析。
研究结果:
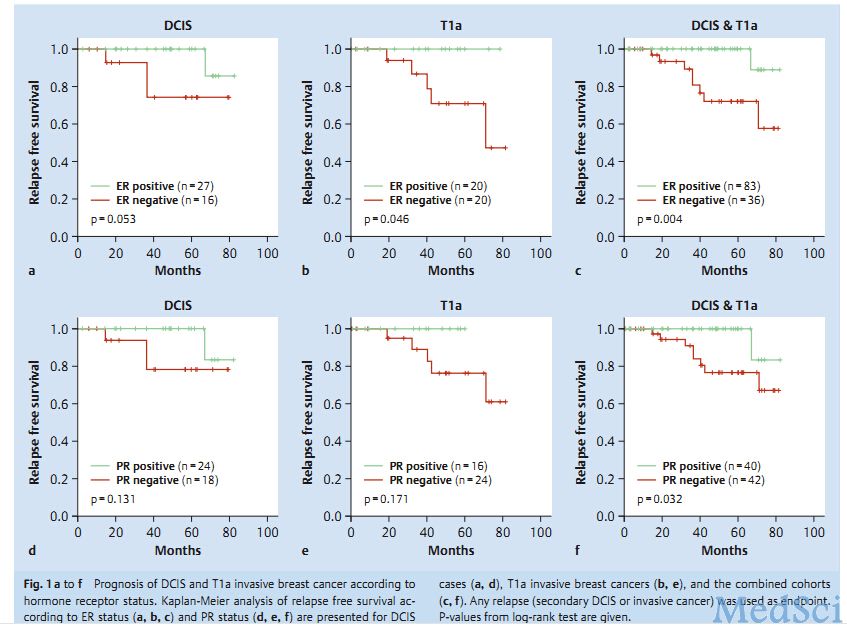
145名患者的临床特征:约1/3为DCIS,中位年龄57岁,大部分患者为ER+,小部分有转移。通过对比DCIS和IBC的各临床病理特征后,并没有发现两组患者在年龄、激素受体、HER2状态、辅助治疗(放疗、内分泌治疗)上的差异。通过分子亚型的比较发现T1aIBC肿瘤比DCIS及其他IBC有更多的的HER2亚型,相比之下luminalHER2型肿瘤比例较少,而在比较骨髓中的DTC后发现DCIS和IBC的DTC并没有统计学差异,在对各临床指标分层后发现PR-与DTC显著相关(Table3)。为评价两组患者的预后有关因素,对43名DCIS和40名T1aIBC患者随访,随访终点为复发。结果发现:中位随访时间DCIS为47个月,T1aIBC为40个月,对各临床因素分层后发现两组无复发生存时间无统计学差异。经过生存分析后发现ER+、PR+患者在两组都在无复发生存上获益(Figa-f)。
研究结论:
导管原位癌和浸润性癌的临床特征并无差异,luminal亚型在DCIS和IBC组都表现出有较好的预后。
原文出处:
Sanger, N., et al., Molecular Markers as Prognostic Factors in DCIS and Small Invasive Breast Cancers. Geburtshilfe Frauenheilkd, 2014. 74(11): p. 1016-1022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#原位癌#
34
#TSH#
37
#评价#
26