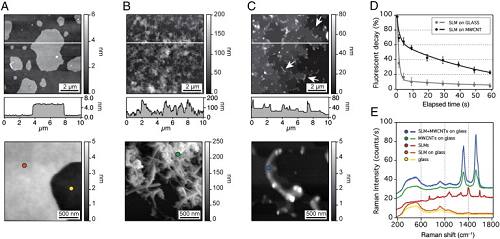
Neuroradiology:3D T2WI 在诊断脊髓硬脊膜动静脉瘘的诊断价值
2017-09-11 shaosai MedSci原创
硬脊膜动静脉瘘(SDAVF)是近20年来才逐渐被人们认识的一种椎管内血管畸形。本研究旨在评价脊髓MRI在有无联合3D T2WI在评价脊髓数字剪影血管造影(DSA)确诊的脊髓SDAVF的价值,并将结果发表在Neuroradiology上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#诊断价值#
39
#静脉#
44
#脊髓硬脊膜#
34
不错的文章.值得一读
63
#3D#
31
#动静脉瘘#
42
#硬脊膜#
31
厉害了--学习了
0
好好文章学习了
64
学习了谢谢分享!!
62