Neurology:见于结节性硬化症的Marcus-Gunn瞳孔
2018-09-04 zyx整理 神经科病例撷英拾粹
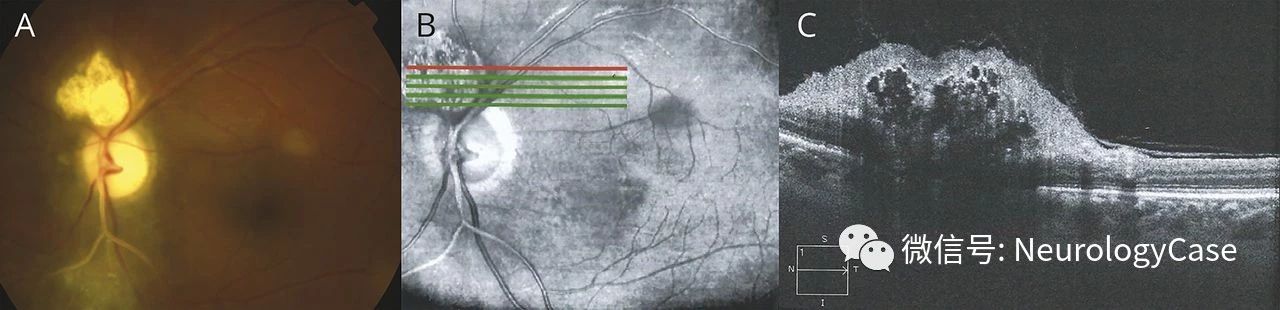
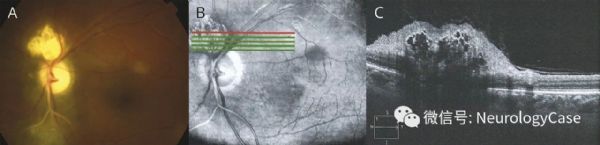
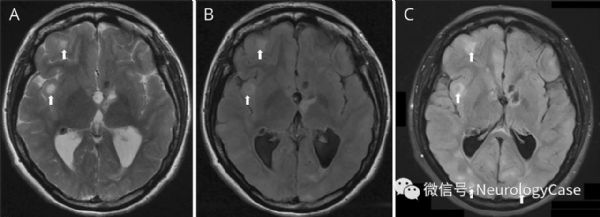
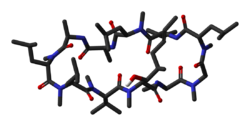
22岁女性,既往有结节性硬化症(TS),行左侧星形细胞瘤不全切除术,表现为视力减退4年。神经系统查体提示左侧相对性传入性瞳孔障碍(RAPD)(视频)伴左侧视盘苍白。双侧视敏度为20/100,左侧上部视野缺损。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#结节性硬化症#
71
#硬化症#
44
#Neurol#
40
#结节性#
46
好
72
#瞳孔#
47
学习谢谢分享
87
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
74
学习
82
谢谢分享,学习了
0