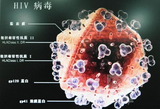
JCI:重大发现!HIV不光以T细胞为靶点,还会靶向作用巨噬细胞
2016-03-11 佚名 不详
图片来源:medicalxpress.com 发表于国际杂志Journal of Clinical Investigation上的一项研究论文中,来自北卡罗来纳州大学医学院的研究人员通过研究发现,HIV可以感染巨噬细胞并在巨噬细胞内进行繁殖,巨噬细胞是机体肝脏、大脑和结缔组织中的一种大型白细胞,该研究发现或可帮助开发治疗HIV感染的新型疗法。 巨噬细胞可以摄入外源性的物质,包括受感染的C

图片来源:medicalxpress.com
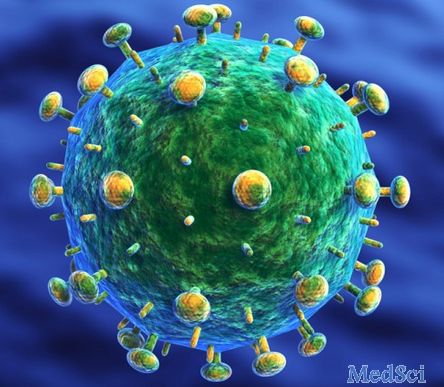
发表于国际杂志Journal of Clinical Investigation上的一项研究论文中,来自北卡罗来纳州大学医学院的研究人员通过研究发现,HIV可以感染巨噬细胞并在巨噬细胞内进行繁殖,巨噬细胞是机体肝脏、大脑和结缔组织中的一种大型白细胞,该研究发现或可帮助开发治疗HIV感染的新型疗法。
巨噬细胞可以摄入外源性的物质,包括受感染的CD4 T细胞,此前很多研究发现,巨噬细胞可以在摄入受损伤的CD4 T细胞后被感染,通过研究没有T细胞的小型动物模型机体的HIV,即细胞足以被HIV感染,研究者发现,HIV感染的巨噬细胞可以证实巨噬细胞热带型HIV菌株的存在,同时病毒还可以自主在巨噬细胞中进行复制。
研究者Joseph Eron博士指出,本文研究明确阐明了巨噬细胞可以作为HIV病毒的复制场所,巨噬细胞是一种髓系细胞,文章中为了确定是否组织中的巨噬细胞可以被HIV感染繁殖,研究者利用一种人源化的髓系小鼠模型进行研究,结果发现,在T细胞不存在的情况下,巨噬细胞可以维持HIV病毒的复制,而HIV感染的巨噬细胞可以分布在机体多个组织中,比如大脑等。具有复制潜能的病毒可以通过来自模型中感染的巨噬细胞来募集,同时受感染的巨噬细胞也可以在新的宿主中建立新型的感染,相关研究结果表明,巨噬细胞或许可以作为HIV感染的真正靶点来维持并且传递这种感染。
如果T细胞是HIV治疗研究中唯一的靶点的话,那么根除病毒似乎并不太可能,如今研究者发现了HIV靶向作用的另一类靶点细胞,这就为有效清理HIV患者的病毒并且开发治疗艾滋病的新型疗法提供了新的思路。如今研究者已经阐明HIV可以靶向作用巨噬细胞并且在巨噬细胞内进行复制,下一步他们将会将抗逆转录病毒疗法引入到模型中来观察是否病毒可以在疗法存在的情况继续进行繁殖。
最后研究者Jenna Bone Honeycutt博士说道,新型模型可以帮助我们提出很多关键问题,比如巨噬细胞是否可以作为患者抗逆转录病毒疗法后的HIV存储库,当然这还需要研究者们进行后期更为深入的研究来进一步阐明其中的机制。
原始出处:
Honeycutt JB, Wahl A, Baker C, Spagnuolo RA, Foster J, Zakharova O, Wietgrefe S, Caro-Vegas C, Madden V, Sharpe G, Haase AT, Eron JJ, Garcia JV.Macrophages sustain HIV replication in vivo independently of T cells. J Clin Invest. 2016 Mar 7. pii: 84456
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#重大发现#
53
#JCI#
31
#靶向作用#
46
厉害
115
应该是哪来的方向
119