Hypertension:高血压和非高血压受试者收缩压与脑灌注的不同关系
2018-11-13 xing.T MedSci原创
然而,在高血压受试者中,似乎存在着SBP中间范围窗,其灌注水平最大。
虽然人们越来越认同高血压与脑血管损害有关,但血压(BP)与脑血流之间的关系尚未完全明确。目前尚不清楚BP处于何种水平以及治疗目标范围对于脑灌注最佳。此外,关于BP如何影响海马灌注的数据有限,海马是一种与记忆密切相关的结构。
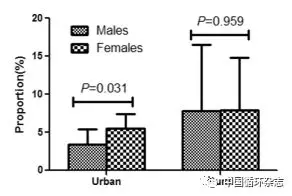
近日,心血管权威杂志Hypertension上发表了一篇研究文章,研究人员对无痴呆或临床表现卒中的老年人进行了横断面(n=445)和纵向(n=185)研究,这些参与者接受了临床检查和脑灌注评估(年龄为69.2±7.5岁,62%为女性,45%为高血压患者)。线性模型用于评估基线BP与血流的关系,并评估BP的变化如何影响灌注的变化。
在整个组中,收缩压(SBP)与大脑皮质(β=-0.13,P=0.005)和海马血流(β=-0.12,P=0.01)呈负相关。值得注意的是,这种负相关性在没有高血压的受试者中较为明显,高血压患者SBP与海马血流呈二元关系(β=-1.55,P=0.03):SBP中位数约125mmHg的参与者灌注最高。纵向地,在高血压受试者中,灌注在低基线SBP时随着SBP的增加而增加,但在高基线SBP时随着SBP的减少而增加。大脑皮质和海马灌注随着SBP的增加而降低。
然而,在高血压受试者中,似乎存在着SBP中间范围窗,其灌注水平最大。
原始出处:
Lidia Glodzik,et al.Different Relationship Between Systolic Blood Pressure and Cerebral Perfusion in Subjects With and Without Hypertension.Hypertension.2018. https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.118.11233
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
30
#脑灌注#
38
#收缩压#
26
#TENS#
34
#非高血压#
28
#受试者#
26
#Hypertension#
25