Autophagy:组蛋白脱乙酰化酶抑制剂可通过FOXO1依赖的途径诱导自噬
2015-05-10 MedSci MedSci原创
自噬是细胞在饥饿、低氧及其他应激状态下,为维持细胞内代谢稳态,而进行的一种分解代谢过程。研究发现,组蛋白脱乙酰化酶抑制剂
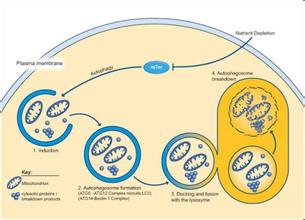
但是,目前关于FOXO1在HDACIs诱导的自噬过程中所起的作用尚无报道。近来,有研究首次分别在mRNA和蛋白水平,证明了HDACIs可以增加FOXO1的表达。同时,还发现HDACIs可以通过增加FOXO1的核聚集和提高FOXO1的转录活性。此外,通过siRNA敲除技术或者特殊的化学抑制剂,可抑制FOXO1的功能,从而显著的抑制HDACIs诱导的细胞自噬。研究者还发现,FOXO1介导的自噬是通过激活FOXO1的转录获得的,最终使诱导细胞自噬表现出双重的效应:1)提高自噬相关基因(ATG)的表达;2)通过SESN3 (sestrin 3)基因的转录抑制MTOR信号途径。最终,研究者发现抑制自噬可以显著提高HDACIs介导的细胞死亡,这提示自噬是有助于细胞存活的重要机制。
综上所述,研究者认为,在HDACIs介导的人类肿瘤细胞的自噬中,FOXO1其非常重要的作用,将HDACIs与自噬抑制剂结合应用,有望成为新型的抗肿瘤治疗策略。
参考文献:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#抑制剂#
36
看看
144
求助这篇文章
109
#组蛋白#
36
#FOXO1#
41