JCO:复旦大学许剑民等发现妥昔单抗联合化疗可有效改善部分结肠癌肝转移患者预后
2013-04-15 JCO dxy
在2013年4月8日在线出版的《临床肿瘤学杂志》(Journal of Clinical Oncology)杂志上,发表了我国复旦大学附属中山医院许剑民副教授等人的一项研究结果,该研究针对无法切除的结肠癌肝转移(CLM)患者,旨在评价西妥昔单抗联合化疗方案用于一线治疗的效果。在该研究中,研究对象为,同时存在无法切除的结肠癌有限肝转移情况的KRAS野生型患者,患者在接受原发肿瘤切除治疗后,经随机分配
在2013年4月8日在线出版的《临床肿瘤学杂志》(Journal of Clinical Oncology)杂志上,发表了我国复旦大学附属中山医院许剑民副教授等人的一项研究结果,该研究针对无法切除的结肠癌肝转移(CLM)患者,旨在评价西妥昔单抗联合化疗方案用于一线治疗的效果。
在该研究中,研究对象为,同时存在无法切除的结肠癌有限肝转移情况的KRAS野生型患者,患者在接受原发肿瘤切除治疗后,经随机分配接受化疗(FOLFIRI [氟尿嘧啶、亚叶酸及伊立替康] 或mFOLFOX6 [改进型氟尿嘧啶、亚叶酸及奥沙利铂])联合西妥昔单抗方案(A组)或单纯化疗方案(B组)治疗。该研究主要终点为,经治疗后肝转移患者可进行手术切除的转化率。次要终点则包括肿瘤缓解率及生存率。
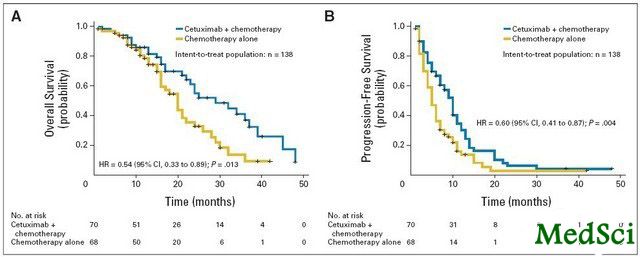
意向治疗人群共有138例患者;其中70例患者被随机分配至A组,68例患者被分配至B组。经过中位时间为25.0个月的随访后发现,全部患者的3年总生存(OS)率及中位生存时间(MST)分别为30%及24.4个月。A组中,肝转移患者R0切除率为25.7% (70例患者中有18 例),B组则为7.4% (68例患者中有5例),组间差异明显(P < .01)。A组患者与B组相比,其客观缓解率得到了改善(57.1% v 29.4%; P < .01),3年OS率得到增加(41% v 18%; P = .013),且MST也得到延长(30.9个月 v 21.0 个月; P = .013)。此外,对于接受肝转移切除治疗的A组患者,与未接受手术治疗的患者相比,其MST明显改善(46.4个月 v 25.7 个月; P < .01)。
许教授等人最后认为,对于起初无法进行切除治疗的KRAS野生型CLM患者,与单纯的化疗方案相比,通过西妥昔单抗联合化疗方案治疗,可提高患者肝转移手术切除可能,并可改善其缓解率及生存率。
与结肠癌相关的拓展阅读:
- JCO:吸烟恶化结肠癌预后
- JBC:研究揭示Pax2在结肠癌中作用机制
- JCO:结肠癌患者久坐可增加死亡风险
- 腰臀比大的人患结肠癌风险增高
- Lancet Oncol:在晚期结肠癌患者中辅助应用贝伐单抗并无益处
- CANCER PREV RES:结肠癌疫苗的小型临床研究中展示明显效果 更多信息请点击:有关结肠癌更多资讯

Randomized Controlled Trial of Cetuximab Plus Chemotherapy for Patients With KRAS Wild-Type Unresectable Colorectal Liver-Limited Metastases.
PURPOSE
To assess the effects of cetuximab plus chemotherapy as first-line treatment for unresectable colorectal liver metastases (CLMs).
PATIENTS AND METHODS
After resection of their primary tumors, patients with KRAS wild-type synchronous nonresectable liver-limited metastases from colorectal cancer were randomly assigned to receive chemotherapy (FOLFIRI [fluorouracil, leucovorin, and irinotecan] or mFOLFOX6 [modified fluorouracil, leucovorin, and oxaliplatin]) plus cetuximab (arm A) or chemotherapy alone (arm B). The primary end point was the rate of patients converted to resection for liver metastases. Secondary end points included tumor response and survival.
Results
The intent-to-treat population comprised 138 patients; 70 patients were randomly assigned to arm A and 68 to arm B. After a median of 25.0 months of follow-up, the 3-year overall survival (OS) rate and median survival time (MST) for all patients were 30% and 24.4 months, respectively. The R0 resection rates for liver metastases were 25.7% (18 of 70 patients) in arm A and 7.4% (five of 68 patients) in arm B, which were significantly different (P < .01). Patients in arm A had improved objective response rates (57.1% v 29.4%; P < .01), increased 3-year OS rate (41% v 18%; P = .013) and prolonged MST (30.9 v 21.0 months; P = .013) compared with those in arm B. In addition, in arm A, patients who had resection of liver metastases had a significantly improved MST (46.4 v 25.7 months; P < .01) compared with those who did not undergo surgery.
CONCLUSION
For patients with initially unresectable KRAS wild-type CLMs, cetuximab combined with chemotherapy improved the resectability of liver metastases and improved response rates and survival compared with chemotherapy alone.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#JCO#
38
#患者预后#
39
#联合化疗#
38
#肝转移#
41
#复旦#
36