INVEST RADIO:钆剂究竟安不安全?对衰老大鼠脑磁共振成像的相关研究
2022-07-13 shaosai MedSci原创
GBCA可在各种组织类型中长期存在,甚至在肾功能正常的健康人中也是如此,这激起了临床实践中对GBCA一般安全性的关注和不确定性。
钆剂(GBCA)在增强磁共振成像(MRI)中的应用已在临床常规中得到证实,在医学成像中具有重要的诊断和预后价值。在过去的十年中,许多临床前和临床研究已经解决了螯合和剂量依赖的因果关系,在齿状核或大鼠小脑深部核团(DCN)和球状核团(GP)的T1加权MRI扫描中显示了GBCA给药和高信号。GBCA可在各种组织类型中长期存在,甚至在肾功能正常的健康人中也是如此,这激起了临床实践中对GBCA一般安全性的关注和不确定性。对于线性结构的GBCAs,研究明确显示,在使用造影剂累积剂量后,平扫T1加权信号强度(SI)和T1缩短会明显持续增加,并导致其在欧盟暂停临床使用。与线性药剂相比,大环GBCAs更加稳定、动力学惰性更高。据报道,大环GBCA在缩短T1方面的结果并不明确,因此需要进一步深入研究。
很少有专门的研究从图像采集到重建的数据变异性明确成像的多种来源,以解决有连续GBCA病史的患者的争议性结果。近日,发表在INVEST RADIO杂志的一项研究通过对大鼠大脑的多参数MRI检查的评估,以全面了解累积性GBCA暴露后定量和半定量MRI SI变化的争议性讨论,并进一步区分了自然的年龄依赖性的MRI参数变化和由于连续使用造影剂而导致的外部驱动,为GBCA的安全应用提供了强有力的数据参考。

25只Wistar-Han大鼠被平均分成5组,最初每周连续4天注射8次3.6毫升/公斤体重的生理盐水(I-III组)或1.8毫摩尔Gd/公斤体重的钆布醇(IV组)或钆双胺(V组)。在最后一次给药后的1周(所有组);5、12、20和26周(生理盐水II、钆布醇、钆双胺);以及35、44和52周(生理盐水III、钆布醇、钆双胺)获得T1和T2加权扫描,以及弛豫map。盐水I在1周后安乐死,盐水II在26周后安乐死,其余各组在52周后安乐死。评估了DCN/Pons(P)和GP/PC的信号强度(SIs),以及DCN和GP的弛豫时间。提取脑组织,并用电感耦合等离子体质谱(ICP-MS)和激光烧蚀-ICP-MS成像对钆、铁和锰的含量进行量化。
T1加权SI比率在任何区域都没有显示出与年龄有关的明显趋势。在52周的组间分析中,钆双胺和其比较者之间的DCN/P和GP/PC区域比率有明显差异。T1松弛时间随着年龄的增长而下降,所有组别在第一次和最后一次测量之间有10%至20%的差异,而在DCN中,仅钆双胺组有10%的明显下降(DCN:P = 0.0158)。在最后一次测量时间点,DCN中钆双胺和生理盐水III(P = 0.0153)以及GP中钆双胺和钆布醇(P = 0.0287)的T1值出现了与组有关的差异。对T2加权图像的SI比值分析显示,随着所有组别年龄的增加,DCN/P的SI比值明显增加,GP/PC的SI比值减少,最后一次注射后52周,各组别之间没有差异。在衰老的大鼠大脑中,GP的T2值随着时间的推移显示出明显的线性下降(盐水I-III:P = 0.0101;钆布醇:P = 0.0001;钆二胺:P = 0.0142)。通过激光烧蚀-ICP-MS对锰和铁的定量成像显示,盐水组在GP中的两种金属(铁:P<0.0001;锰:P=0.0306)和DCN中的锰(P=0.0187)均呈线性增长,但在52周时组间无差异。
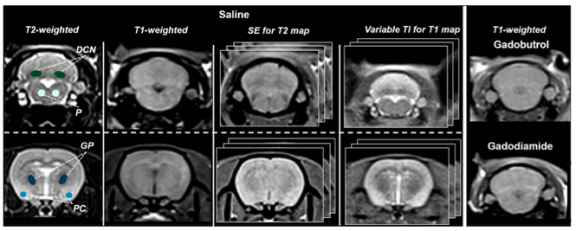
图 第1-4栏:在最后一次盐水注射后1周,大鼠在盐水I中的代表性MRI扫描,具有示范性的ROI划分(T2 map的回波时间为8.5毫秒;T1 map的反转时间为200毫秒)。第5列:小脑深部核团(DCN)区域的钆布醇和钆双胺动物的代表性T1加权图像
本研究发现,大鼠GP的T1和T2值表现出与年龄相关的下降。此外,本研究还发现DCN/P的T2加权SIR增加,而GP/PC的SIR则随时间推移而减少。因此,在评估MRI SIRs或弛豫测量数据作为大脑中存在钆的替代物时,必须将年龄视为一个混杂因素。此外,本研究长期MRI分析显示,在连续应用大环螯合GBCA钆丁醇后,齿状核和GP没有钆沉积。与我本研究MRI结果一致,体外金属定量显示,在1年的观察期内Gd免疫动物的铁浓度明显增加,在研究结束时,各组之间没有明显的差异。
原文出处:
Claudia Green,Gregor Jost,Thomas Frenzel,et al.The Effect of Gadolinium-Based Contrast Agents on Longitudinal Changes of Magnetic Resonance Imaging Signal Intensities and Relaxation Times in the Aging Rat Brain.DOI:10.1097/RLI.0000000000000857.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#相关研究#
39
#钆剂#
45
#EST#
33
#磁共振#
55