Clin Cancer Res:帕博利珠单抗新辅助和辅助治疗可切除局部晚期头颈部鳞状细胞癌患者的疗效
2022-03-08 yd2015 MedSci原创
可切除局部晚期的头颈部鳞状细胞癌(HNSCC)患者,尽管进行了辅助(化疗)放疗,但1年无病生存期(DFS)率为65% - 69%。近期,Clin Cancer Res杂志上发表了一项II期研究成果,主
可切除的局部晚期头颈部鳞状细胞癌(HNSCC),术后进行辅助化疗或联合放疗后,1年无病生存期(DFS)率仅为65% - 69%。因此,寻找提高术后DFS率的治疗方案势在必行。近期,Clin Cancer Res杂志上发表了一项II期研究成果,主要是评估Pembrolizumab(帕博利珠单抗)新辅助和辅助治疗可切除局部晚期头颈部鳞状细胞癌患者的疗效。
患者术前1-3周接受Pembrolizumab(帕博利珠单抗)200mg治疗,术后根据切缘阳性与否分为中风险和高风险患者,术后均接受放疗(60–66 Gy)和同步pembrolizumab (每3周一次,共6周期)。高风险患者还同期接受每周顺铂 (40 mg/m2 )。主要研究终点为1年DFS率。次要终点为1年总生存率(OS)和病理缓解(PR)。使用CTCAE v5.0标准进行安全性评估。
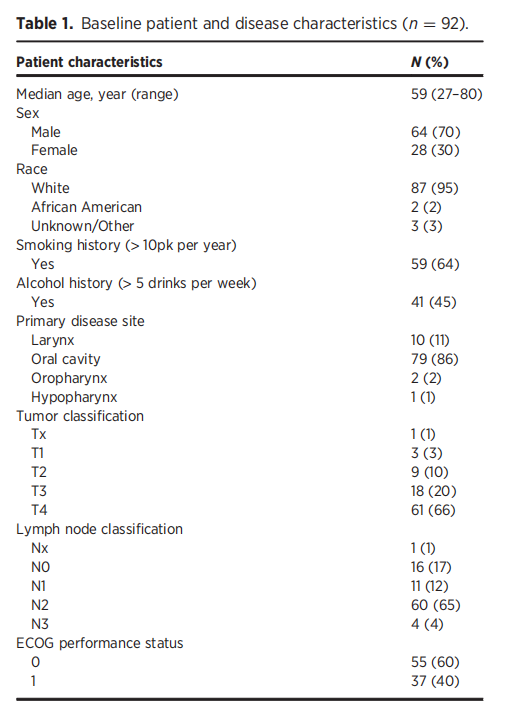
2016年2月至2020年10月,共纳入92例患者。中位年龄为59岁(范围27 - 80岁),30%为女性,86%为T3 - T4期,69%为N2期。
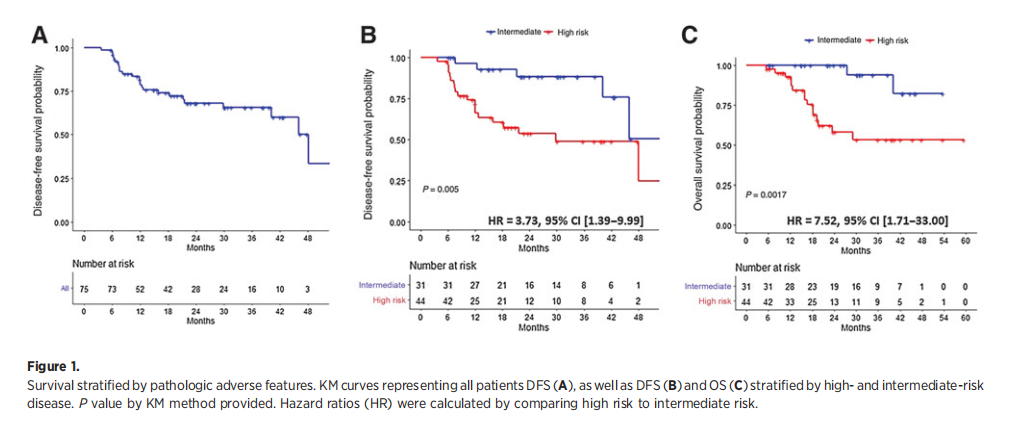
在所有可评估患者(n=75)中位随访28个月时,1年DFS率为80% (95% CI, 71%-90%),其HR为0.60 (95% CI, 0.39 -0.93;P=0.0233),与RTOG 9501研究的整个队列相比显著更高。中危组(n=31) 1年DFS率为96% (95% CI, 90%-100%)。显著高于RTOG 9501研究中仅接受放疗治疗的中危组患者,其1年DFS率为69% (95% CI, 59% 78%) (P=0.0007),其危险比为0.23 (95% CI, 0.09-0.58;P=0.0018)。相比之下,高危组的1年DFS率为66% (95% CI, 55%-84%),这与RTOG 9501研究中进行放化疗治疗的患者类似(65%;95%CI, 57% -64%),HR=0.86 (95% CI, 0.52 1.44;P =0.5736)。
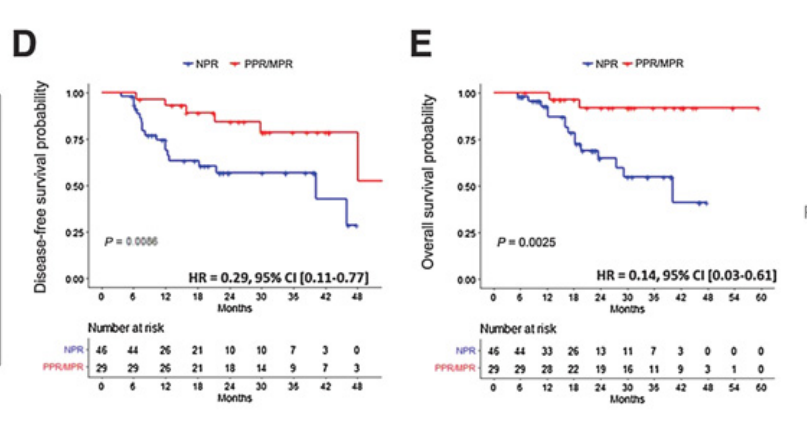
可评估患者的PR为39%,MPR为7%。中危患者的PR(55%)高于高危患者的PR率(28%)。重要的是,获得PR患者与无PR患者相比,1年DFS率显著增加,分别为93% (95% CI, 84% -100%)比72% (95% CI, 59%- 87%)(P=0.0086);两组的OS也有显著差异[100% (95% CI, 100% 100%) vs. 93% (95% CI, 85% 100%),P= 0.004]。
没有新的安全信号。. 3级TRAE发生在15例中危组患者中(36%)和32例高风险组患者中(64%)。

综上,研究表明,Pembrolizumab(帕博利珠单抗)新辅助和辅助治疗可提高中危患者的1年DFS率。
原始出处:
Trisha M. Wise-Draper, Shuchi Gulati1 , Sarah Palackdharry, et al. Phase II Clinical Trial of Neoadjuvant and Adjuvant Pembrolizumab in Resectable Local–Regionally Advanced Head and Neck Squamous Cell Carcinoma. Clin Cancer Res 2022;doi: 10.1158/1078-0432.CCR-21-3351.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#细胞癌#
59
#局部晚期#
44
#帕博利珠#
32
#新辅助#
38
#头颈部鳞状细胞癌#
36
#局部#
39
#头颈部#
38
#颈部#
36