为提高肿瘤的治疗效果,临床上多采用两种或两种以上药物联合的化疗方案。然而联合用药在提高疗效的同时可能会因为药物之间的相互作用或者抗癌药物作用的周期特异性对化疗的疗效和毒性产生影响,并且临床实践中亦存在忽略用药顺序的现象,因此正确的给药顺序是肿瘤合理用药的重要组成部分。
化疗方案的给药顺序应遵循以下3个原则:
相互作用原则:
化疗药物之间发生相互作用时,应注意给药的先后顺序,将可能发生的不良反应降至最低。如紫杉醇和顺铂,顺铂会延缓紫杉醇的排泄,加重不良反应的发生,联用时须先给予紫杉醇。
细胞动力学原则:
生长较慢的实体瘤处于增殖期的细胞较少,G0期细胞较多,先用周期非特异性药物杀灭一部分肿瘤细胞,使肿瘤细胞进入增殖期再用周期特异性药物。而生长快的肿瘤先用周期特异性药物大量杀灭处于增殖周期的细胞,减少肿瘤负荷,随后用周期非特异性药物杀灭残存的肿瘤细胞。
刺激性原则:
使用非顺序依赖性化疗药物时,应先用对组织刺激性较强的药物,后用刺激性小的药物。由于治疗开始时静脉尚未损伤,结构稳定性好,药液渗出机会少,药物对静脉引起的不良反应较小如长春瑞滨和顺铂合用时,长春瑞滨刺激性强,宜先给药。
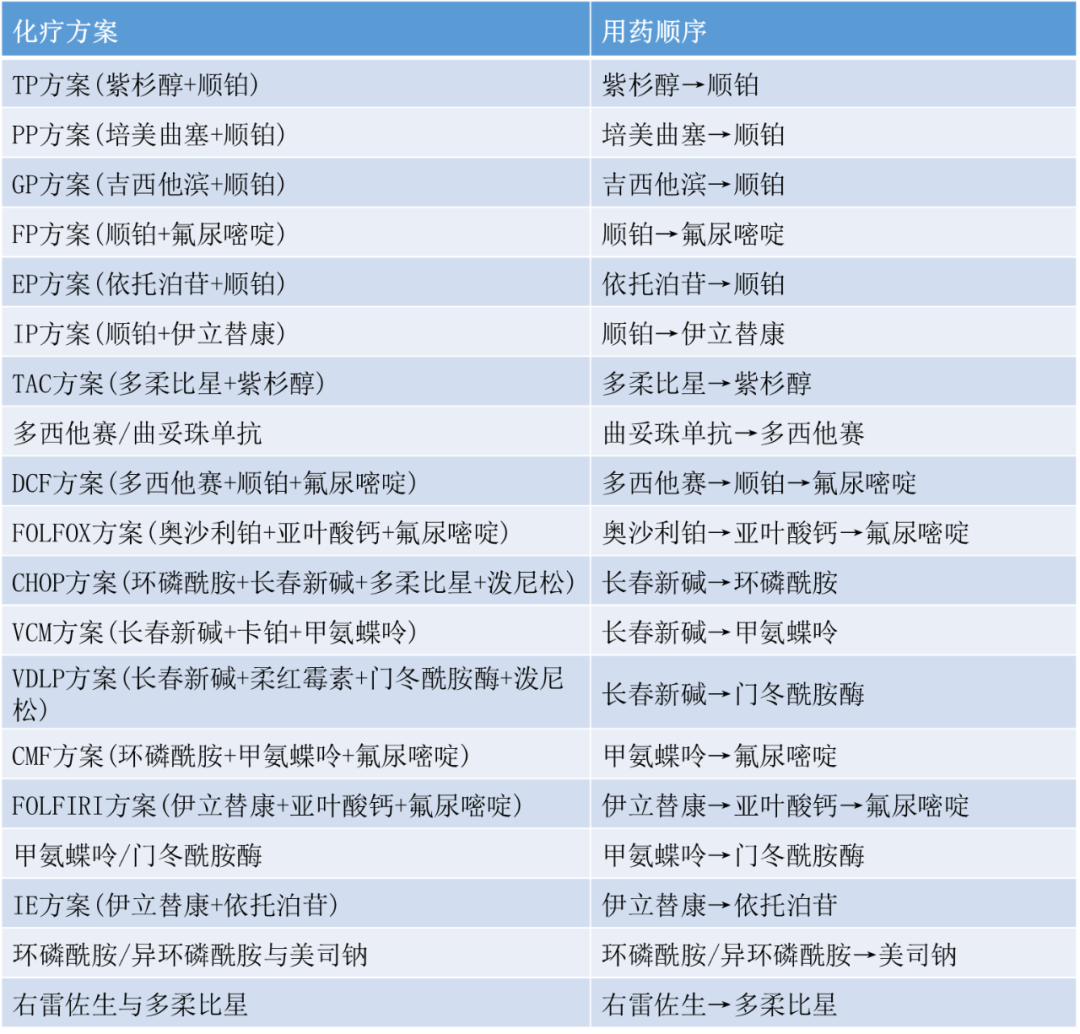
常见不同癌症联合化疗方案的用药顺序
1、TP 方案(紫杉醇+顺铂)
用药顺序:紫杉醇→顺铂
当顺铂在紫杉醇之前给药时,AUC平均最低值大于相反顺序给药的AUC,说明机体对前一种情况的清除率较低。紫杉醇和顺铂联合给药顺序依赖性的研究,提示当使用一些能调整P450酶代谢作用或由P450所代谢的药物,与紫杉醇联用,可能引起紫杉醇滞留体内,提高机体中毒的可能性。顺铂对细胞色素P450酶有抑制作用,使紫杉醇的清除率降低30%。
2、PP 方案(培美曲塞+顺铂)
用药顺序:培美曲塞→顺铂
培美曲塞导致嘌呤和嘧啶合成障碍,使细胞分裂停止在 S 期,然后再用细胞周期非特异性的顺铂杀灭残存的肿瘤细胞。而先用顺铂会导致培美曲塞的肾脏排泄减慢,相关毒副作用会增加。
3、GP 方案(吉西他滨+顺铂)
用药顺序:吉西他滨→顺铂
顺铂会影响吉西他滨体内过程,加重骨髓抑制。而吉西他滨可抑制顺铂引起的 DNA 损伤的修复、增加双链的断裂和顺铂-DNA 复合物的形成,此外,先给予吉西他滨再给顺铂时,不良反应发生率也较低。
4、FP 方案(顺铂+氟尿嘧啶)
(用药顺序:顺铂→氟尿嘧啶)
Koizumi W 等进行了一项比较顺铂和氟尿嘧啶不同用药顺序对化疗有效性和安全性影响的临床试验,结果显示虽没有统计学差异,但 A 组(顺铂→氟尿嘧啶)患者总体有效率(31.3%)、中位总生存期(239d)、疾病进展时间(175d)相对于 B 组(氟尿嘧啶→顺铂)患者的 13.9%、174d、140d 更高,并且两组患者不良反应发生率没有统计学差异。
从药效学上分析,顺铂可增加细胞内四氢叶酸生成,提高细胞对氟尿嘧啶的敏感性,起到协同作用。故先给予顺铂具有更好的抗肿瘤活性作用。
5、EP 方案(依托泊苷+顺铂)
用药顺序:依托泊苷→顺铂
依托泊苷(细胞周期特异性药物)与拓扑异构酶 II,抑制有丝分裂,使细胞分裂停止于 S 期或 G2 期,然后再用顺铂(细胞周期非特异性药物)杀灭残存的肿瘤细胞。
6、IP 方案(顺铂+伊立替康)
用药顺序:顺铂→伊立替康
Ⅱ期临床试验表明,顺铂在伊立替康之前给药有较高的有效率,先给顺铂,可增加伊立替康活性代谢产物 SN-38的清除率,降低严重恶心呕吐、腹泻、骨髓抑制的发生率,提高化疗有效率。
7、TAC 方案(多柔比星+紫杉醇)
用药顺序:多柔比星→紫杉醇
紫杉醇与多柔比星通过共同途径代谢,相互竞争代谢途径,当紫杉醇与多柔比星联合使用时,可能会提高多柔比星及其活性代谢物的血药浓度。紫杉醇在多柔比星之前给药时,发生的中性粒细胞减少和口腔炎更重。
8、多西他赛/曲妥珠单抗
用药顺序:曲妥珠单抗→多西他赛
多西他赛与曲妥珠单抗联用时,多西他赛首次静脉给药应于曲妥珠单抗第 1次用药后1天;如果患者对前次曲妥珠单抗剂量耐受良好,多西他赛以后的用药应紧随曲妥珠单抗静脉输注之后。
9、DCF 方案(多西他赛+顺铂+氟尿嘧啶)
用药顺序:多西他赛→顺铂→氟尿嘧啶
临床试验证明多西他赛和顺铂之间没有药动学相互作用,但研究结果显示先用多西他赛较先用顺铂的化疗方案可能有更低的毒性和不良反应发生率。
另外,临床试验表明,顺铂在氟尿嘧啶之前用药组,总体有效率、中位总生存期、疾病进展时间均优于氟尿嘧啶在顺铂之前用药组。小剂量顺铂能够增加细胞内蛋氨酸,使细胞内活性叶酸生成增加,从而增加氟尿嘧啶的抗肿瘤作用。
10、FOLFOX 方案(奥沙利铂+亚叶酸钙+氟尿嘧啶)
用药顺序:奥沙利铂→亚叶酸钙→氟尿嘧啶
亚叶酸钙是四氢叶酸的 5-甲酰衍生物,可增加四氢叶酸的浓度,与氟尿嘧啶产生协同作用;另外,奥沙利铂为细胞周期非特异性药物,杀灭肿瘤细胞的同时,驱动 G0 期细胞进入增殖周期,再使用作用于 S 期的氟尿嘧啶,产生协同作用。若先使用氟尿嘧啶,奥沙利铂会降低其清除率,增加其骨髓抑制等毒性。
11、CHOP 方案(环磷酰胺+长春新碱+多柔比星+泼尼松)
用药顺序:长春新碱→环磷酰胺
Razek A 等对长春新碱和环磷酰胺联合用药时的给药顺序和间隔进行了体外研究,结果表明同时给药并没有显示出相加作用,随着给药时间间隔的延长,相加作用出现,先给予长春新碱可能具有更好的抗肿瘤活性。
长春新碱具有同步化作用,使肿瘤细胞停滞在 M期,约 6-8小时后细胞同步进入 G1期,此时用环磷酰胺可增加疗效;另一方面长春新碱可能增加肿瘤细胞的通透性,提高细胞内环磷酰胺浓度,产生更强的抗肿瘤作用。
12、VCM 方案(长春新碱+卡铂+甲氨蝶呤)
用药顺序:长春新碱→甲氨蝶呤
长春新碱可阻止甲氨蝶呤从细胞内渗出,提高后者的细胞内浓度,故先给予长春新碱,再用甲氨蝶呤,可增加疗效。
13、VDLP 方案(长春新碱+柔红霉素+门冬酰胺酶+泼尼松)
用药顺序:长春新碱→门冬酰胺酶
长春新碱与门冬酰胺酶合用,可能增强神经系统及血液系统的障碍。为将毒性控制到最小,可将硫酸长春新碱在门冬酰胺酶给药前12-24小时使用。
14、CMF 方案(环磷酰胺+甲氨蝶呤+氟尿嘧啶)
用药顺序:甲氨蝶呤→氟尿嘧啶
甲氨蝶呤可阻断嘌呤合成,增加磷酸核糖焦磷酸钠(PRPD)含量,PRPD 为活化氟尿嘧啶所必须物质,因此应先给甲氨喋呤,4-6小时后再给予氟尿嘧啶,否则会减效。
15、FOLFIRI 方案(伊立替康+亚叶酸钙+氟尿嘧啶)
用药顺序:伊立替康→亚叶酸钙→氟尿嘧啶
该方案是治疗晚期结肠癌(ACC)的常用方案。亚叶酸钙是氟尿嘧啶的增效剂,联合使用可提高氟尿嘧啶的疗效。氟尿嘧啶在体内代谢为脱氧氟尿嘧啶核苷酸,它可结合并抑制胸苷酸合成酶(该酶在DNA修复和复制中十分重要)。亚叶酸在体内转化成 5,10-亚甲基四氢叶酸,该转化物能够稳定脱氧氟尿嘧啶核苷酸与胸苷酸合成酶的结合,进而增强氟尿嘧啶对该酶的抑制作用。因此,先给予亚叶酸钙,可以使氟尿嘧啶抑制胸苷酸合成酶作用时间延长,增加疗效。若亚叶酸钙在氟尿嘧啶之后给药,则无法起到增效的作用。
有研究发现,给予伊立替康后再用CF及氟尿嘧啶,伊立替康的中间体SN-38的AUC较之相反顺序下降约40%,且不良反应的发生率更低,同时患者的耐受性增加。
16、甲氨蝶呤/亚叶酸钙
用药顺序:甲氨蝶呤→亚叶酸钙
亚叶酸钙是叶酸体内的活化形式,甲氨蝶呤作为一种叶酸还原酶抑制剂,主要通过拮抗叶酸发挥细胞毒作用,联用时若先给予亚叶酸钙,甲氨蝶呤疗效降低,而应用大剂量甲氨蝶呤后用亚叶酸钙起到解毒作用。
17、甲氨蝶呤/门冬酰胺酶
用药顺序:甲氨蝶呤→门冬酰胺酶
门冬酰胺酶与甲氨蝶呤一起用时,可通过抑制细胞复制的作用而阻断甲氨蝶呤的抗肿瘤作用。据相关研究,在给甲氨蝶呤后24小时内应用门冬酰胺酶,可以避免产生抑制甲氨蝶呤的抗肿瘤作用,并可减少甲氨蝶呤对胃肠道和血液系统的不良反应。
18、IE 方案(伊立替康+依托泊苷)
用药顺序:伊立替康→依托泊苷
拓扑异构酶 I 抑制剂伊立替康能够增加拓扑异构酶 II 抑制剂依托泊苷的敏感性,增加了细胞内拓扑异构酶 IImRNA 的含量,使其过表达,增强依托泊苷的抗肿瘤作用。
19、环磷酰胺/异环磷酰胺与美司钠
用药顺序:环磷酰胺/异环磷酰胺→美司钠
美司钠在大剂量环磷酰胺(>10mg/kg)/异环磷酰胺使用同时、使用后 4 h、8 h 给药,美司钠可以与 CTX 和 IFO 的肾脏代谢产物结合从而降低两者的膀胱毒性。
20、右雷佐生与多柔比星
用药顺序:右雷佐生→多柔比星
右雷佐生为 EDTA 的环状衍生物,容易穿透细胞膜。实验研究表明,右雷佐生在细胞内转变为开环螯合物,干扰铁离子中介的自由基形成,而后者为蒽环类药物产生心脏毒性的部分原因。故不得在右雷佐生使用前给予多柔比星。
总结
目前对于化疗联合用药顺序的研究还不尽成熟,期待着更多关于用药顺序的临床试验及循证依据出现,以上整理的资料希望能对临床有益,能促进肿瘤合理用药,以免发生严重的非预期不良反应。
来源 | e药安全、肿瘤时间、人卫药学
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












感谢,已学
32
#化疗#
91
已经学习了
41
打卡学习了
55
#化疗药#
49
感谢分享
48