A&R:男性系统性硬化症患者患癌风险高
2013-08-15 0906siyu dxy
男性肿瘤SSc患者肿瘤发生率高于女性,而所有癌症的总体SIR是1.41(95%可信区间[95%CI]:1.18-1.68) 来自日本神户大学医学院的Akira Onishi等人进行了一项研究,作者通过荟萃分析以人群为基础的队列研究,来确定系统性硬化症(SSc)患者的癌症发生率。研究结果在线发布在2013年7月的《关节炎与风湿病》(ARTHRITIS & RH
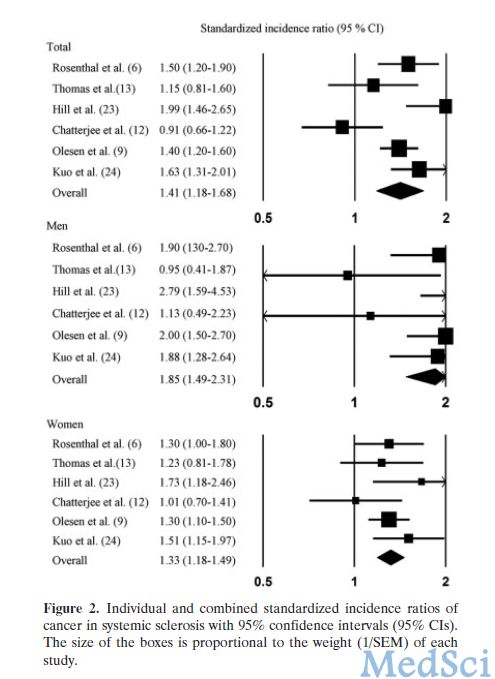
男性肿瘤SSc患者肿瘤发生率高于女性,而所有癌症的总体SIR是1.41(95%可信区间[95%CI]:1.18-1.68)
来自日本神户大学医学院的Akira Onishi等人进行了一项研究,作者通过荟萃分析以人群为基础的队列研究,来确定系统性硬化症(SSc)患者的癌症发生率。研究结果在线发布在2013年7月的《关节炎与风湿病》(ARTHRITIS & RHEUMATISM)杂志上。作者发现,虽然绝对风险相对较低,但是SSc患者肿瘤发生风险高,特别是肺癌、肝癌、血液系统肿瘤和膀胱癌。男性SSc患者肿瘤的发生率高于女性。【原文下载】
数据来源于五种不同的数据库(Medline, Scopus, CINAHL[护理和联合卫生文献累积索引], Web of Science和Cochrane协作网),文献发布时间设置为1966年1月至2012年5月。搜索到的综述性文章及其参考文献列表也在评价范围中。与确定SSc患者癌症风险相关,且是以人群为基础的队列研究数据被纳入该研究。研究者对所有满足严格筛选表针的文章数据,包括人口规模、随访时间和观察到预期的癌症率,即标准化的发病率(SIRs)进行分析。
研究结果如下:该meta分析共纳入6篇符合标准的文章。所有癌症的总体SIR是1.41(95%可信区间[95%CI]:1.18-1.68)。研究的参与者、结局、研究设计和偏倚风险作为结果的可变性,存在显著的异质性。男性的总体SIR(1.85 [95%CI:1.49-2.31])显著高于女性(SIR 1.33 [95%CI:1.18-1.49])。针对性别分层后能消除异质性,这一结果揭示,该研究的差异是由性别差异造成的。皮肤局限型SSc和皮肤弥漫型SSc之间无显著差异。SSc患者肺癌、肝癌、血液系统肿瘤、膀胱癌、及非霍奇金淋巴瘤和霍奇金淋巴瘤的风险显著升高。
研究发现,虽然绝对风险相对较低,但是SSc患者患肿瘤风险高,特别是肺癌、肝癌、血液系统肿瘤和膀胱癌。男性SSc患者肿瘤的发生率高于女性。
原始出处:
Onishi A Sugiyama D Kumagai S Morinobu A.Cancer incidence in systemic sclerosis: meta-analysis of population-based cohort studies.Arthritis Rheum 2013 Jul 65 7 :1913-21. 【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#系统性#
32
#癌风险#
28
#硬化症#
36
#患癌风险#
32
#患癌#
38
#系统性硬化#
28