J Clin Oncol:PI3Kδ/CK1ε双重抑制剂Umbralisib用于治疗复发性/难治性惰性淋巴瘤
2021-03-09 Nebula MedSci原创
Umbralisib是一种PI3Kδ/CK1ε的双重抑制剂,用于治疗复发性/难治性惰性淋巴瘤如何呢?
磷脂酰肌醇-3-激酶(PI3K)抑制剂在复发性或难治性(R/R)惰性非霍奇金淋巴瘤(iNHL)中显示出治疗活性。PI3K抑制剂的长期耐受性差,毒性大,影响其持续使用。Umbralisib是一种PI3Kδ/CK1ε的双重抑制剂,与其他PI3K抑制剂相比,它对PI3Kδ具有更高的选择性。
这项IIb期试验旨在评估Umbralisib用于R/R iNHL患者的疗效和安全性。
这是一项多队列、开放标签的IIb期研究,招募了208名对既往治疗(包括≥1抗CD20为基础的治疗)无效的R/R边缘区、滤泡性或小淋巴细胞性淋巴瘤 (MZL、FL或SLL) 患者,每天予以Umbralisib 800mg口服,直到疾病进展、不可耐受的毒性或撤出研究。主要终点是总体应答率;次要终点包括反应时间、反应持续时间、无进展生存期和安全性。
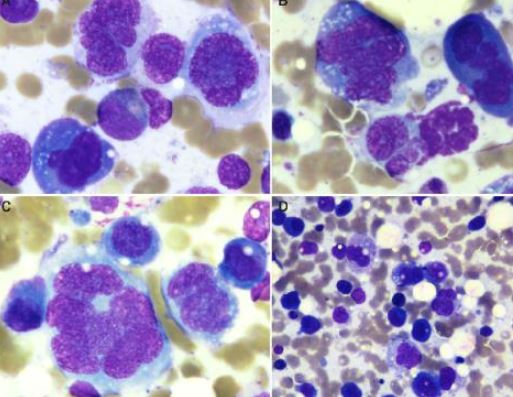
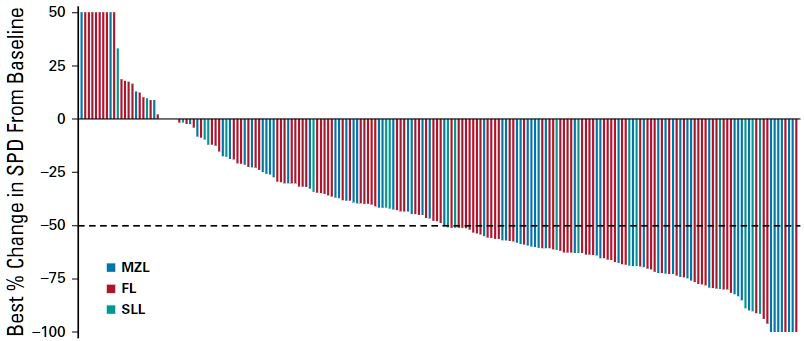
指数病变大小的反应
中位随访时间为27.7个月(有效性分析)和21.4个月(安全性分析)。总有效率为47.1%,86.4%的患者的肿瘤可观察到缩小。中位有效时间为2.7~4.6个月。MZL、FL和SLL患者的中位缓解期分别为未达到、11.1个月和18.3个月。MZL、FL和SLL的中位无进展生存期分别为未到达、10.6个月和20.9个月。
DOR和PFS
53.4%的患者至少报告了一种3级及以上的需紧急治疗的不良事件(TEAE)。TEAE导致32例(15.4%)患者停用Umbralisib。共有31名患者(14.9%)因治疗相关的不良事件而停止治疗。发生于10%及以上患者的3级及以上TEAE有:中性粒细胞减少(11.5%)和腹泻(10.1%)。ALT/AST升高(≥3级)的发生率为6.7%/7.2%。
综上,Umbralisib在严重预处理的iNHL患者中取得了有意义的临床活性。安全性可控,免疫介导的毒性和不良事件相关停药的发生率相对较低。
原始出处:
Fowler Nathan H,Samaniego Felipe,Jurczak Wojciech et al. Umbralisib, a Dual PI3Kδ/CK1ε Inhibitor in Patients With Relapsed or Refractory Indolent Lymphoma. J Clin Oncol, 2021, undefined: JCO2003433.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#抑制剂#
25
#Oncol#
29
#复发性#
28
#PI3Kδ#
34
#PI3K#
44
#Umbralisib#
29
#难治性#
27
治疗淋巴瘤
64
谢谢梅斯分享这么多精彩信息
41