Circulation:保守治疗还是侵入性治疗?慢性冠心病患者的选择因人而异
2022-03-18 网络 网络
基线心绞痛更频繁的患者在接受侵入性策略治疗时,QOL的症状、身体功能和心理健康方面有更大的改善,而基线有罕见/不存在的心绞痛的患者没有报告与治疗相关的QOL差异
慢性稳定性冠心病的诊断有两个要求:第一,有明确的冠心病诊断:(1)有心肌梗死病史;(2)冠状动脉造影证实有冠状动脉狭窄≥50%;(3)无创检查证实有冠状动脉狭窄或心肌缺血证据;第二,临床表现为无心绞痛症状的冠心病患者或稳定性心绞痛患者,即60 d内心绞痛发作频率、持续时间、诱因或缓解方式无变化。心绞痛同时不伴有心肌损伤的证据(心肌酶升高)。冠状动脉痉挛导致的静息心绞痛也归属于此类范畴。
慢性稳定性冠心病在冠心病中占绝大多数,如何管控这一患者群体,减少他们的心血管事件发生,已成为医务工作者的重要工作。为此,来自美国杜克大学的专家开展了相关研究,旨在评估此类患者最佳的治疗方式,结果发表在Circulation杂志上。

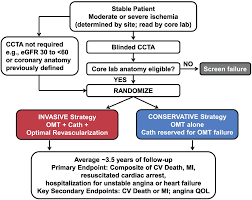
ISCHEMIA试验对5179名患有慢性冠心病(CCD)和中度或重度缺血的参与者进行了初始侵入性治疗策略(INV)和初始保守性策略(CON)的比较。在1819名参与者中(907名INV,912名CON),在基线、随机化后3、12、24和36个月以及研究结束时通过结构化访谈收集了一系列疾病特异性和通用的QOL工具。评估包括与心绞痛相关的QOL(SAQ-19)、一般健康状况(EQ-5D)、抑郁症状(患者健康问卷-8),以及北美患者的心脏功能状况(DASI)。
结果显示,纳入的参与者中位年龄为67岁,19.2%为女性,15.9%为非白人。SAQ-19总结得分的估计平均差异有利于INV(1.4分,95% CI:0.2-2.5在所有随访中)。在基线心绞痛罕见/不存在的患者中(SAQ心绞痛频率[AF]得分>80)没有观察到差异。
在基线心绞痛较为频繁的患者中(SAQ AF得分≤80,744名患者,41%),随机接受INV治疗的患者的SAQ-19总结得分平均比CON高3.7分(95%CI:1.6-5.8),在SAQ各分量表上的效果一致。身体限制3.2分(95% CI 0.2, 6.1),心绞痛频率3.2分(95% CI 1.2, 5.1),生活质量/健康认知5.3分(95% CI 2.8, 7.8)。
对于DASI,总体上没有因治疗而产生差异,但在基线SAQ房颤得分≤80的患者中,INV的DASI得分较高(3.2分,95%CI 0.6,5.7),而基线心绞痛罕见/不存在的患者没有显示出与治疗相关的差异。中度至重度抑郁症在随机化时并不常见(11.5%-12.8%),并且不受治疗分配的影响。
在ISCHEMIA综合QOL分项研究中,基线心绞痛更频繁的患者在接受侵入性策略治疗时,QOL的症状、身体功能和心理健康方面有更大的改善,而基线有罕见/不存在的心绞痛的患者没有报告与治疗相关的QOL差异。
参考文献:
Comprehensive Quality of Life Outcomes with Invasive versus Conservative Management of Chronic Coronary Disease in ISCHEMIA. https://doi.org/10.1161/CIRCULATIONAHA.121.057363. Circulation. 2022;0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#侵入性#
57
谢谢分享。
50
#冠心病患者#
55
#保守治疗#
43