Sci Rep:全新设备使癌细胞“无所遁形”,轻松发现早期癌症!
2017-07-18 Heather_z727 来宝网
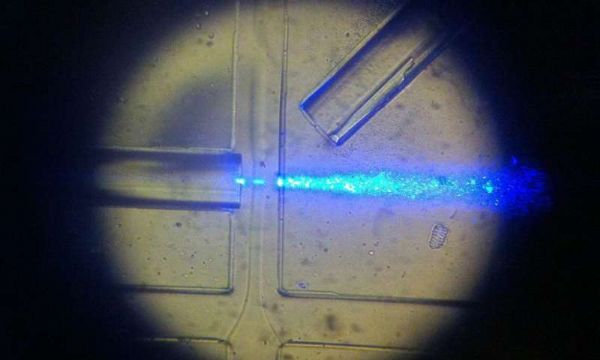
癌症的检测一直是困扰医生的方法之一,检测过程不仅复杂,还会对患者造成伤害,近日,来自URV的研究人员开发出一种无机化学专利便携设备,可以检测出血液中的肿瘤细胞,这种设备可以计算血液样本中肿瘤细胞的数量,因此可以实时高效的提高监测,治疗和诊断的癌症的效率。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新设备#
41
#早期癌症#
46
优秀
63
#癌细胞#
33