JACC:睡眠不足,肚子变大,增加多种疾病风险,即使补觉也难以逆转
2022-03-29 生物世界 生物世界
从长远来看,这些发现提示了睡眠不足是导致肥胖、心血管疾病和代谢疾病流行的原因之一。
睡眠不足往往是一种行为选择,而且,现在这种选择越来越普遍。熬夜已经成为许多年轻人的“新常态”。据世界卫生组织(WHO)的统计,全球睡眠障碍率达27%,而在中国,成年人失眠发生率高达38.2%,六成以上90后觉得睡眠不足,也就是说,有超过3亿中国人存在睡眠障碍,而且这一数据还在逐年上升中。
这些睡眠不足,有部分原因是因为工作的原因,但还有相当一部分原因是人们在本该睡眠的时间里使用手机等智能设备。睡眠不足,意味着醒着的时间更多,这也导致了吃得更多,而且这些多出来的醒着的时间里往往不会增加身体活动。
近日,美国梅奥医学中心的研究人员在《美国心脏病学会杂志》(JACC)发表了题为:Effects of Experimental Sleep Restriction on Energy Intake, Energy Expenditure, and Visceral Obesity 的研究论文。
这项随机交叉对照临床试验发现,睡眠不足会增加热量摄入,而热量消耗却几乎没变化,这导致体重轻微增加,却显著增加内脏脂肪的堆积。
这表明睡眠不足是之前未被认识到的触发内脏脂肪堆积的新因素,而补觉在短时间内并不能逆转之前因睡眠不足导致的内脏脂肪积累。
研究队列由12名不肥胖的健康人组成(9名男性,3名女性,年龄在19-39岁之间),所有人均经历两个21天的实验周期,21天分为4天适应期、14天实验期、3天恢复期。
在前4天的适应期,所有人均每晚睡9小时,接下来的14天,所有人随机分配到睡眠限制组(4小时睡眠)和睡眠对照组(9小时睡眠),接下来是3天恢复期,所有人每晚睡9小时。三个月后,所有参与者分配到相反的组,再进行一次21天周期。
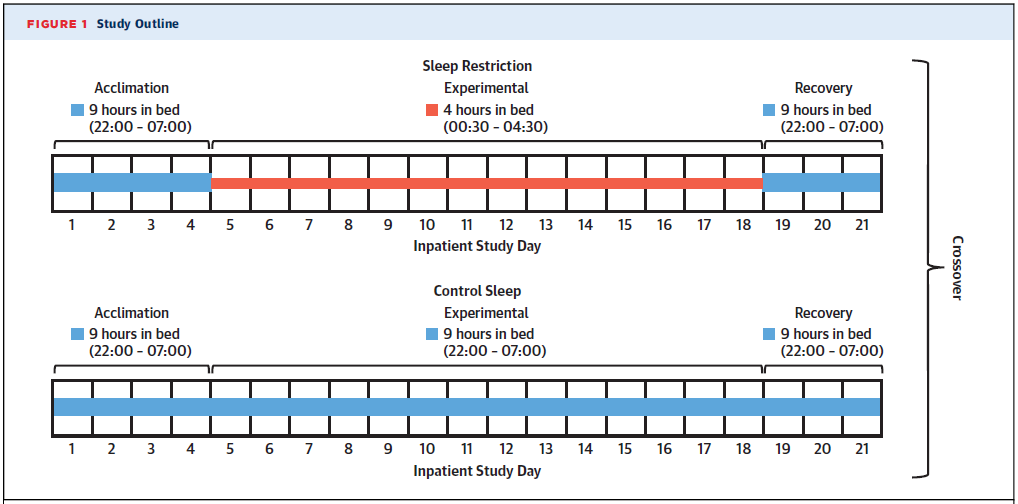
在整个研究过程中,每组都可以自由选择食物。研究人员同时监测他们的能量摄入、能量消耗、体重变化、脂肪分布(包括内脏脂肪或腹部脂肪)等。
与适应期相比,参与者在睡眠限制期每天多消耗约308千卡的额外热量,摄入的蛋白质和脂肪增加了约13%和17%。在睡眠限制的早期热量摄入增加最多,然后在恢复期逐渐减少到起始水平。
总体来讲,整个过程中能量消耗则基本保持不变。也就是说,睡眠减少的过程中,能量摄入有所增加,但能量消耗却基本保持不变。检测结果显示,在此期间,体重只有轻微增加(约0.5公斤),如果只测量体重,看起来睡眠不足并没什么问题。
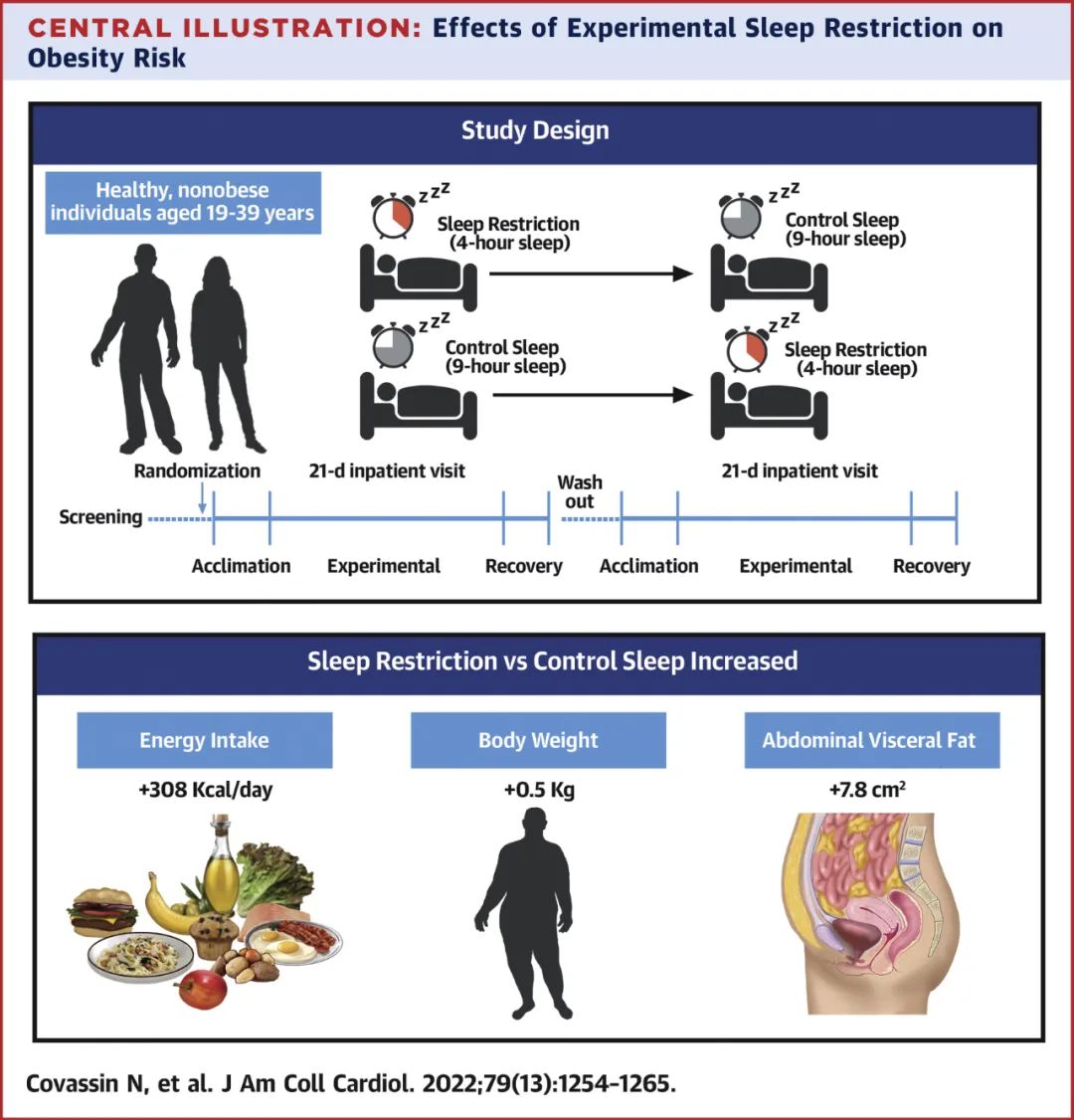
然而,研究人员通CT扫描检测了参与者的腹部脂肪和内脏脂肪变化。结果显示,睡眠不足导致腹部总脂肪增加9%,腹部内脏脂肪增加11%。
该研究的通讯作者 Virend Somers 教授表示,这项研究结果显示,即使是年轻、健康,而且相对较瘦的人,睡眠时间缩短后,也会导致热量摄入增加、体重上升,尤其是腹部脂肪堆积显著增加。
Virend Somers 教授进一步指出,通常情况下,脂肪会优先堆积到皮下。然而,在睡眠不足的情况下,脂肪会优先堆积到内脏器官周围,这种情况更为危险。更重要的是,此时即使恢复正常的睡眠时间,热量摄入和体重会随之减少,但内脏脂肪却仍在继续增加。
这些发现表明,睡眠不足是之前未被认识到的触发内脏脂肪堆积的新因素,而补觉在短时间内并不能逆转之前因睡眠不足导致的内脏脂肪积累。
研究团队指出,这项研究表明,那些经常睡眠不足的人,会逐渐积累内脏脂肪,这显然具有和拿的潜在风险。而对于那些因工作导致睡眠不足的人,需要考虑通过其他方式干预来抵抗内脏脂肪堆积,例如增加运动锻炼、选择更健康的食物等等。
从长远来看,这些发现提示了睡眠不足是导致肥胖、心血管疾病和代谢疾病流行的原因之一。
论文链接:
Effects of Experimental Sleep Restriction on Energy Intake, Energy Expenditure, and Visceral Obesity.JACC.https://doi.org/10.1016/j.jacc.2022.01.038
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JACC#
0
#补觉#
51
#ACC#
34
#疾病风险#
39
学习了,有用
51
内容很好
45