JAMA Oncol:子宫肌瘤切除术后潜在的癌症
2015-02-23 赵洲 MedSci原创
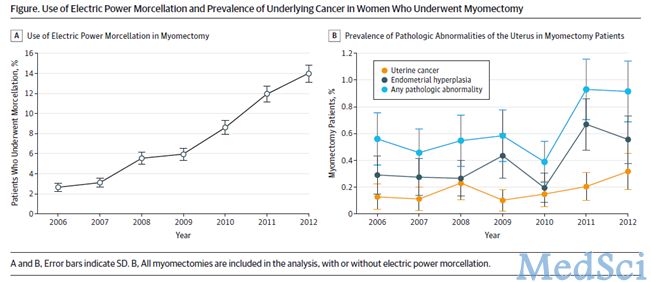
子宫肌瘤是子宫中的良性平滑肌瘤。这些肌瘤是很常见的,据估计20%-50%女性有子宫肌瘤。尽管子宫肌瘤通过是无症状的,但能造成疼痛、月经不调以及生育能力降低。子宫肌瘤切除术现在常常通过微创手术得以实现。电动分碎术,或者使用机械装置切除子宫肌瘤有可能被用于促进子宫肌瘤的切除。为了分析潜在的癌症和癌症前期变化的患病率,研究人员使用了美国国家数据库进行回顾性分析。数据是在2006年1月至2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Oncol#
23
#切除术#
33
很不错学习了
134
#子宫肌瘤切除术#
33
好文章,超赞
76
感谢你们的辛勤付出
175
不错的文章,学习了
112