窄 QRS 波心动过速:这些鉴别诊断方法不可不知
2016-12-21 心血管时间 心血管时间
窄 QRS 波心动过速一般为 QRS 时间 ≤ 0.10 s、心率>100 次/min 的心动过速,绝大多数窄 QRS 波心动过速为室上性心动过速,但也包括少数分支型室速也表现为窄 QRS 波心动过速。分类1. 原发性房性心律失常:窦房结折返性心动过速(SNRT)、心房扑动(AFL)以及心房颤动(AF)、房内折返性心动过速(IART)、自律性房速(AAT)、多源性房性心动过速(MAT)等。2. 折
窄 QRS 波心动过速一般为 QRS 时间 ≤ 0.10 s、心率>100 次/min 的心动过速,绝大多数窄 QRS 波心动过速为室上性心动过速,但也包括少数分支型室速也表现为窄 QRS 波心动过速。
分类
1. 原发性房性心律失常:窦房结折返性心动过速(SNRT)、心房扑动(AFL)以及心房颤动(AF)、房内折返性心动过速(IART)、自律性房速(AAT)、多源性房性心动过速(MAT)等。
2. 折返性心动过速(包括房室结以及旁路):房室结折返性心动过速(AVNRT),房室折返性心动过速(AVRT)。
鉴别诊断
1. 心率:
房速的频率通常为 100~220 次/min,房扑的心房频率为 250~350 次/min,二者皆有重合,临床上如果心动过速时心率在 150 次/分左右,首先要想到房扑 2:1 的可能,并注意观察 II III aVF 是否存在大锯齿波,是否有等电位线,临床上予以鉴别。
2. P 波与 QRS 波之间的关系(即 PR 间期与 RP 间期的比例):
在心动过速中,如果能识别 P 波将有助于诊断。根据 P 波位置又分为:
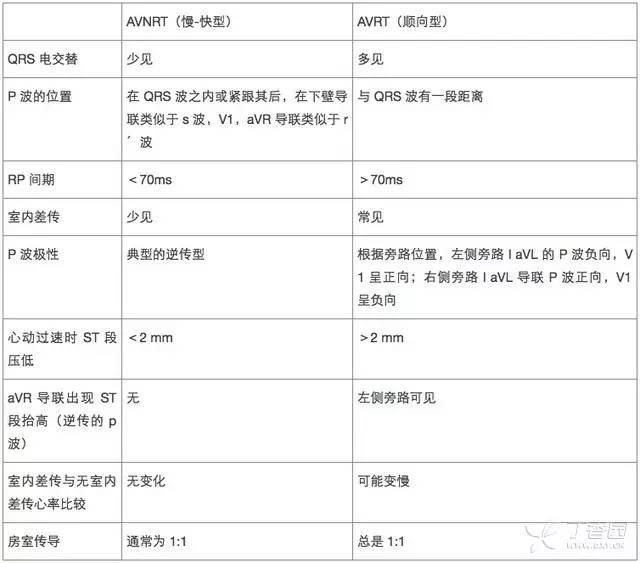
① RP 间期<PR 间期常为 AVNRT 以及 AVRT。在 AVNRT 中 P 波的位置在 QRS 波内或者紧跟其后,在 II III aVF 导联会出现类似于 s 波,在 aVR,V1 导联会出现类似于 r'波,并且此时若 RP 间期>70ms,多数为 AVRT 若 ≤ 70ms,则 AVNRT 可能性大;
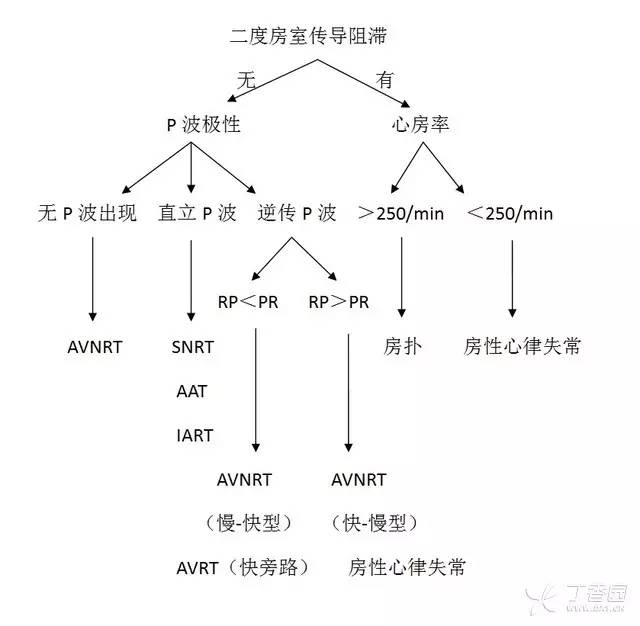
② 若 RP 间期>PR 间期则需要考虑为房速,非典型的 AVNRT(快慢型),以及慢旁路参与的 AVRT。若无 P 波可见首先要想到心房纤颤的可能,具体观察 RR 间期是否匀齐:若匀齐,则是否有大锯齿波即 FL 波,若无则为 AVNRT 的可能。因在 AVNRT 的 P 波多为逆传型,半数隐藏于 QRS 中不得辨认,半数紧接 QRS 波之后出现,在下壁导联酷似 s 波。具体详见下表 1:

3. 电交替:
在心动过速发生的过程中动作电位间期交替导致特殊传导系统相对不应期的摆动会引起 QRS 波电交替,此项指标与心率及心动过速的类型均有关系,只作为参考,若在无房室传导阻滞的窄 QRS 波心动过速出现 QRS 波电交替提示为 AVRT,但也有时可见于心率很快的 AVNRT 中。
4. 房室传导阻滞:
若窄 QRS 波心动过速发生房室传导阻滞者可以排除 AVRT 以及 AVNRT,多数为房性心律失常,若心率在 150 次/min 的心动过速,首先要想到房扑 2:1 的可能,需要仔细辨认是否存在锯齿波,也可以通过刺激迷走神经的方法进一步显露扑动波予以鉴别,具体详见下表 2:
相关心律失常的主要鉴别点
1. 房颤与房扑:
在房扑呈等比例下传过程中 RR 间期匀齐,与房颤较容易鉴别,但当房扑以非等比例下传过程中,RR 间期不齐,但房扑有明显的扑动波,呈锯齿状,而房颤为小细颤波,在心率上房扑的心房率为 250~350 次/min,而房颤要快则在 350~600 次/min 之间,临床上二者不难鉴别。
2. 房速与房室结折返性心动过速(AVNRT):
① 房速若起源于高位心房,P 波直立,而 AVNRT/AVRT 多为房室结逆传 P 波倒置;
② 房速的 P 波多位于 QRS 波之前,PR 间期<RP 间期,而常见的慢-快型 AVNRT 则 RP 间期<PR 间期;
③ 若发生房室传导阻滞后,则基本不会出现 AVNRT 及 AVRT,则多为房性心律失常;
④ 若心动过速发作开始时出现「温醒现象」,提示房速;
⑤房速的 PP 间期由于房速的频率以及房室结的传导时间的原因可以不固定,而 AVNRT 的 RP 间期固定。
3. 房室折返性心动过速(AVRT)与房室结折返性心动过速(AVNRT)
二者鉴别主要在假性 r'波与假性 s 波和 RP 间期等鉴别,详见下表 3:
4. 慢-快型与快-慢型房室结折返性心动过速
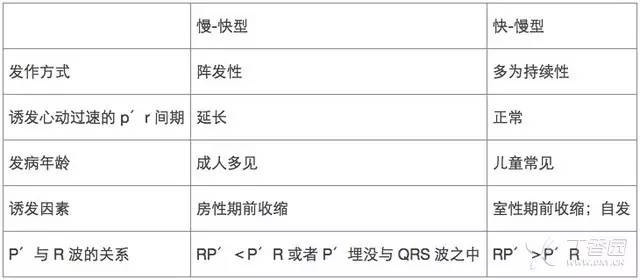
房室结折返性心动过速即房室结内存在传导速度以及不应期相差的两种径路,当一个房早抵达房室结时,慢径路已经脱离不应期,激动延慢径路缓慢下传,到达交接区远端时,快径路已经脱离不应期,激动可延快径路逆传心房。
根据前向传导通路可分为 3 种类型慢快型、快慢型、慢慢型。而慢-快型则为常见类型,而快-慢型则通过快径路下传,慢径路逆传,临床少见,二者鉴别如下表 4:
临床上窄 QRS 波心动过速常见,对于窄 QRS 波心动过速的鉴别也尤为重要,在临床中一旦出现窄 QRS 波心动过速,要想到所有可能的情况,并根据其体表心电图特点加以鉴别,并行电生理检查予以诊断。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#诊断方法#
46
#心动过速#
34
#鉴别诊断#
24
文章很好,值得学习
67
多谢,又再次总结了一遍
63
心电图好难
56