JAHA:绝经后妇女组胺H2受体拮抗剂与心力衰竭风险之间的关系
2022-02-24 MedSci原创 MedSci原创
临床H2RA的使用与绝经后妇女的HF事件无关。未来的研究需要根据性别、HF严重程度或使用模式对H2RA暴露和HF风险的潜在影响进行评估。
根据2013年至2016年的数据,估计有620万20岁以上的美国人被诊断出患有心力衰竭(HF),其中320万是女性。2014年,在55岁的女性中,估计有504000例新诊断的心力衰竭病例。既往的研究表明,在相对较小的研究中,与H2受体拮抗剂(H2RA)非使用者相比,服用H2RA的个体发生心力衰竭(HF)的风险较低。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员在大规模女性健康倡议(WHI)研究中评估了H2RA使用与绝经后女性心衰事件之间的相关性。
这项研究纳入了来自WHI研究的绝经后妇女,她们在基线时没有HF病史。HF被定义为首次因HF住院并经医生裁定的HF事件。在调整人口统计学、生活方式和病史变量后,多变量Cox比例风险回归模型评估了H2RA使用作为时变暴露与HF风险之间的关联。敏感性分析评估了(1)根据ARIC(社区动脉粥样硬化风险)评分分层的HF风险,(2)H2RA使用的倾向评分匹配,(3)使用质子泵抑制剂而不是未服用H2R者作为对照人群,以及(4)排除那些在基线时服用利尿剂的参与者。该研究的主要分析纳入经过排除标准筛查后的158854名女性,其中9757名(6.1%)参与者服用H2RA。
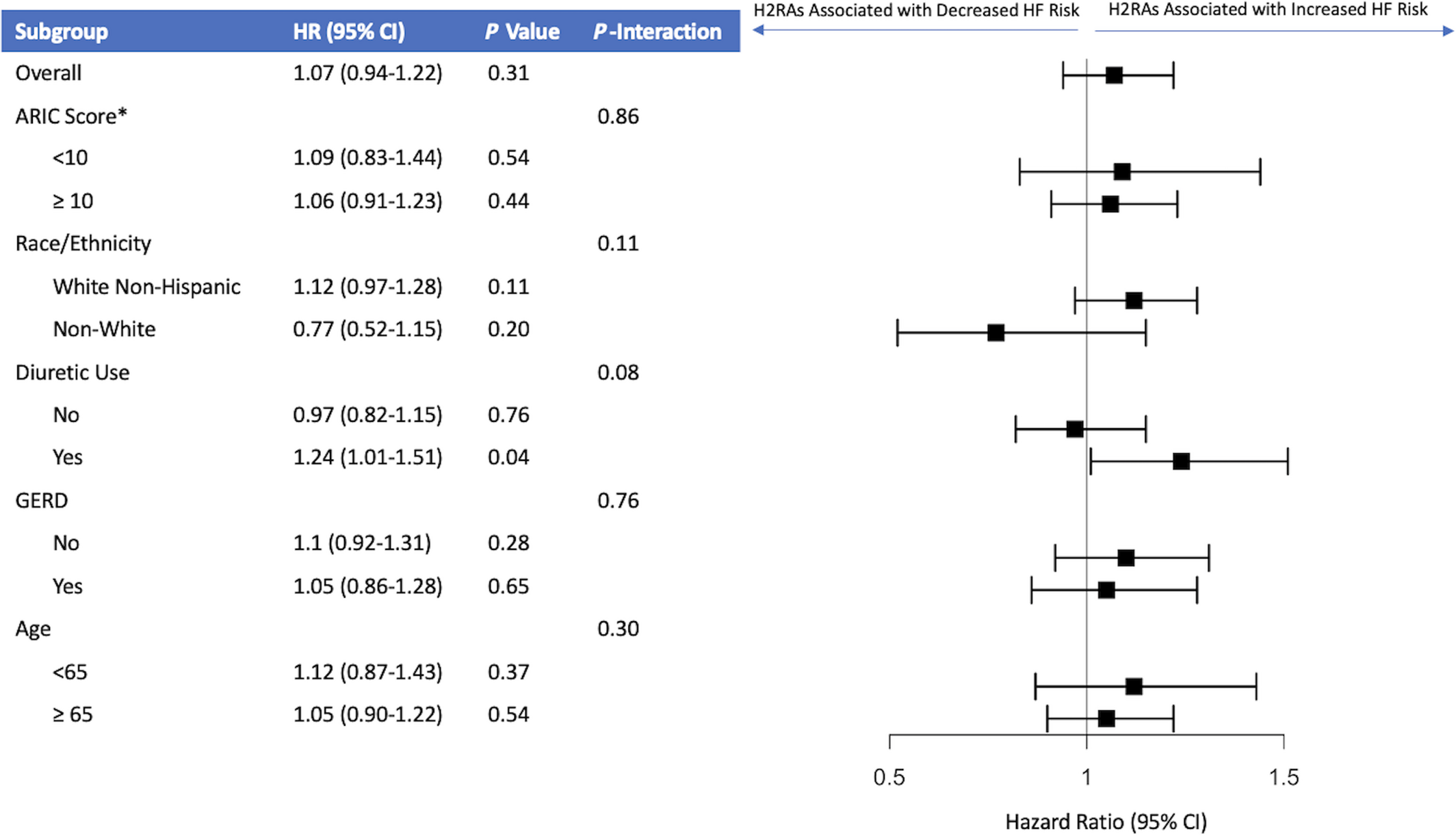
在中位8.2年的随访期间,376名H2RA使用者(4.9次事件/1000人年)和3206名非使用者(2.7次事件/1000人年)发生心衰。多变量调整后,在主要分析(风险比为1.07;95%CI为0.94-1.22;P=0.31)或任何敏感性分析中,H2RA的使用与HF之间没有关联。
由此可见,临床H2RA的使用与绝经后妇女的HF事件无关。未来的研究需要根据性别、HF严重程度或使用模式对H2RA暴露和HF风险的潜在影响进行评估。
原始出处:
Sophia R. Larson.et al.Histamine H2 Receptor Antagonists and Heart Failure Risk in Postmenopausal Women: The Women’s Health Initiative.JAHA.2022.https://www.ahajournals.org/doi/10.1161/JAHA.121.024270
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#组胺#
40
#绝经#
39
#AHA#
33
#绝经后妇女#
44
#拮抗剂#
64
#绝经后#
35
不错,很受用
59
1
63