Lancet Haematology:阿仑单抗治疗T细胞大颗粒淋巴细胞性白血病患者可减少毒性
2015-12-17 崔倩 译 MedSci原创
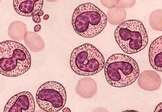
T细胞大颗粒淋巴细胞性白血病(T-LGL)是一种淋巴增生性疾病,特点是免疫介导的血细胞减少和细胞毒性CD3+CD8+ 淋巴细胞克隆扩增。使用甲氨蝶呤,环孢素,或环磷酰胺作为第一治疗可改善50%患者的血细胞减少问题,但长期使用这些药物可导致中毒。研究人员的目的是探索阿仑单抗的活性和安全性,这是一种抗T-LGL患者CD52单克隆抗体。研究人员做了一项单臂,2期临床试验,该研究连续纳入T-LGL成人患者
T细胞大颗粒淋巴细胞性白血病(T-LGL)是一种淋巴增生性疾病,特点是免疫介导的血细胞减少和细胞毒性CD3+CD8+ 淋巴细胞克隆性扩增。使用甲氨蝶呤、环孢素或环磷酰胺作为第一治疗可改善50%患者的血细胞减少问题,但长期使用这些药物可导致中毒。研究人员的目的是探索阿仑单抗的活性和安全性,这是一种抗T-LGL患者CD52单克隆抗体药物。
研究人员做了一项单臂、2期临床试验,该研究连续纳入T-LGL成人患者,在美国马里兰州贝塞斯达美国国立卫生研究院进行。阿仑单抗静脉给药,每天10mg,为期10天。主要终点是在注射后3个月的血液学反应。一个完整的反应被定义为所有受影响的细胞的正常化,部分反应被定义为在中性粒细胞减少的患者中绝对中性粒细胞增加100%,数量大于5×10^8个细胞/L,并在那些贫血患者中,如在两个间隔1周的连续检测中血红蛋白增加20g/L或更高,并且持续1个月或更长的时间,而没有外源性生长因子支持或输血。采用意向性治疗进行分析。研究人员报告了这个两阶段试验的第一阶段的成果;第二阶段继续进行招募。
从2006年10月1日到2015年3月1日,研究人员招募了25例T-LGL患者。14例(56%;95%Cl 35-76)在3个月时有血液学反应。4例有相关骨髓增生异常综合征的患者和2例接受造血干细胞移植的患者没有反应或没有进行评估,这意味着19例患者中的14例(74%[49-91])有经典的T-LGL反应。所有的患者(24[96%]例患者1-2级,1例[4%]患者3级)都有输液反应,这改善了对症疗法。所有患有淋巴细胞减少的患者,22(88%)例患者有3或4级淋巴细胞减少事件发生。其他最常见的3级和4级不良事件是白细胞减少(8[32%])和中性粒细胞减少感染(5[20%])。7例死亡;都是无反应患者。
这是对阿仑单抗治疗T-LGL患者最大和唯一的前瞻性研究。这种在主要是复发和难治性疾病的患者中的淋巴细胞毒性药物一个疗程的活性报告,建议可以通过不继续使用的口服免疫抑制剂来实现血液学反应。
原始出处:
Bogdan Dumitriu,Sawa Ito,Xingmin Feng,et al.Alemtuzumab in T-cell large granular lymphocytic leukaemia,Lancet Haematology,2015.12.16
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Lancet#
20
#细胞性#
30
#HAE#
35
#阿仑单抗#
31
增加知识
127
好文章,值得看。
97
#淋巴细胞#
29
#EMA#
26