Pediatrics:产妇肥胖或易致孩子自闭
2012-04-20 刘鹏 新华网
近日,国际杂志《儿科》Pediatrics看刊登了美国的一项最新医学研究结果,结果显示,与体重正常的产妇相比,肥胖产妇的孩子可能更容易患自闭症和出现生长发育迟缓症状。 列数字 按照4月9日发布的研究报告,研究团队由美国加利福尼亚大学戴维斯分校学者葆拉·克劳科维亚克领导,以加利福尼亚州1004名、年龄在2岁至5岁之间的儿童为对象,发现517人患自闭症谱系障碍、即广义自闭症,172人生长发育迟缓。

近日,国际杂志《儿科》Pediatrics看刊登了美国的一项最新医学研究结果,结果显示,与体重正常的产妇相比,肥胖产妇的孩子可能更容易患自闭症和出现生长发育迟缓症状。
列数字
按照4月9日发布的研究报告,研究团队由美国加利福尼亚大学戴维斯分校学者葆拉·克劳科维亚克领导,以加利福尼亚州1004名、年龄在2岁至5岁之间的儿童为对象,发现517人患自闭症谱系障碍、即广义自闭症,172人生长发育迟缓。
自闭症谱系障碍患儿中,48人的母亲患妊娠期糖尿病,111人的母亲体型肥胖,148人的母亲有高血压等涉及新陈代谢的症状。
发育迟缓的儿童中,20人的母亲患妊娠期糖尿病,41人的母亲体型肥胖,60人的母亲有关联新陈代谢的病症。
研究人员推断,儿童患自闭症与产妇有妊娠期糖尿病之间关联不大,而产妇体型肥胖或有涉及新陈代谢的症状与儿童患自闭症相关联,婴儿生长发育迟缓则关联产妇肥胖、妊娠期糖尿病和新陈代谢问题。
探原因
自闭症主要特征包括漠视情感、拒绝交流和语言发育迟滞,症状一般在儿童3岁前即有所表现。自闭症谱系障碍是广义自闭症,依据典型自闭症核心特征扩展定义。
克劳科维亚克说,一些研究结果显示,肥胖产妇关联血管的病症和体内炎症蛋白过多可能影响胎儿大脑发育。
另外,一些学者说,孕妇患糖尿病易导致对胎儿供氧不足,同时可能降低胎儿体内铁元素含量,影响胎儿大脑发育。
克劳科维亚克的研究团队认为,最新研究结果无法证明产妇肥胖一定导致婴儿患自闭症,但即使只是表明一种可能性也足以引起大家重视。
发呼吁
按照克劳科维亚克研究团队的调查结果,美国育龄女性近6成体重超标,三分之一体型肥胖,16%患以高血压、胰岛素抵抗等为特征的新陈代谢综合征。
美国疾病控制和预防中心不久前发布的一份报告显示,美国每88名儿童中有1人患自闭症谱系障碍,患病比例比2006年增加大约25%。
克劳科维亚克说,无法断言儿童患自闭症的比例上升关联育龄女性肥胖率,只是,两者同时上升的状况应该引起大家关注。另外,出于自身健康考虑,孕妇也应该避免肥胖。
美国迈阿密大学神经学者汉娜·加德纳部分认同克劳科维亚克的说法:无论那两项比率是否存在必然联系,人们都应鼓励准妈妈们为了宝宝的健康而远离肥胖。(生物谷Bioon.com)

doi:10.1542/peds.2011-2583
PMC:
PMID:
Maternal Metabolic Conditions and Risk for Autism and Other Neurodevelopmental Disorders
Paula Krakowiak, MSa,b, Cheryl K. Walker, MDc, Andrew A. Bremer, MD, PhDd, Alice S. Baker, BAa, Sally Ozonoff, PhDb,e, Robin L. Hansen, MDb,f, and Irva Hertz-Picciotto, PhDa,b
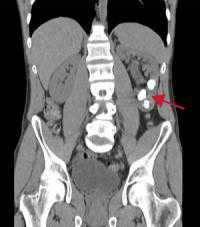
OBJECTIVE: We examined whether metabolic conditions (MCs) during pregnancy (diabetes, hypertension, and obesity) are associated with autism spectrum disorder (ASD), developmental delays (DD), or impairments in specific domains of development in the offspring. METHODS: Children aged 2 to 5 years (517 ASD, 172 DD, and 315 controls) were enrolled in the CHARGE (Childhood Autism Risks from Genetics and the Environment) study, a population-based, case-control investigation between January 2003 and June 2010. Eligible children were born in California, had parents who spoke English or Spanish, and were living with a biological parent in selected regions of California. Children’s diagnoses were confirmed by using standardized assessments. Information regarding maternal conditions was ascertained from medical records or structured interview with the mother. RESULTS: All MCs were more prevalent among case mothers compared with controls. Collectively, these conditions were associated with a higher likelihood of ASD and DD relative to controls (odds ratio: 1.61 [95% confidence interval: 1.10–2.37; odds ratio: 2.35 [95% confidence interval: 1.43–3.88], respectively). Among ASD cases, children of women with diabetes had Mullen Scales of Early Learning (MSEL) expressive language scores 0.4 SD lower than children of mothers without MCs (P < .01). Among children without ASD, those exposed to any MC scored lower on all MSEL and Vineland Adaptive Behavior Scales (VABS) subscales and composites by at least 0.4 SD (P < .01 for each subscale/composite). CONCLUSIONS: Maternal MCs may be broadly associated with neurodevelopmental problems in children. With obesity rising steadily, these results appear to raise serious public health concerns.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
34
#Pediatric#
34
#DIA#
36
#自闭#
37