虽然疾病调整疗法(disease modifying therapy,DMT)的使用改变了缓解-复发型多发性硬化症(RRMS)患者的长期预后,但在治疗继发性进展型多发性硬化症(SPMS)时,其前景却更加谨慎。然而,临床医生需要考虑治疗SPMS患者,特别是当有证据表明有明显的炎症活动时。
十多年来,一种有可能减轻长期残疾的新疗法首次被授权用于治疗SPMS。在EXPAND试验中,西波尼莫德( siponimod)。它是一种选择性的刺丝氨酸-1-磷酸调节剂,可降低残疾累积的风险,尤其是在进入研究前2年内复发的患者。
最近来自MSBase的一项观察性研究显示,如果持续治疗,SPMS患者和有发作性炎症证据的患者(但没有)的残疾累积较慢。因此,临床试验的证据和登记资料都表明,对于活动性SPMS患者,免疫治疗是有必要的。在实现这些益处方面,高疗效治疗是否优于低疗效治疗还不确定。
如果不考虑治疗效果的延迟,即所谓的治疗滞后(therapeutic lag),可能会掩盖治疗效果,特别是在残疾可能性较高的患者的队列中。一些队列和注册数据已经充分证明了观察性数据在分析治疗结果方面的效用。
藉此,墨尔本大学的Izanne Roos等人利用The MSBase registry数据,在考虑到治疗滞后的情况下,比较了高疗效和低疗效疗法在减轻活动性和非活动性SPMS患者残疾恶化和复发方面的有效性。
他们从MSBase和OFSEP这两个大型观察队列中选取了SPMS发病后接受高疗效(纳他利珠单抗、阿莱木单抗、米托蒽醌、奥克雷珠单抗、利妥昔单抗、克拉霉素、芬戈莫德)或低疗效(β干扰素、醋酸格拉替雷、特立氟胺)治疗的患者。根据每一位患者的人口和临床特征,对其治疗滞后进行了估计。倾向性评分(Propensity score)被用来匹配接受高疗效和低疗效治疗的患者。在配对的、成对删减的分析中比较了不考虑治疗滞后期后的结果。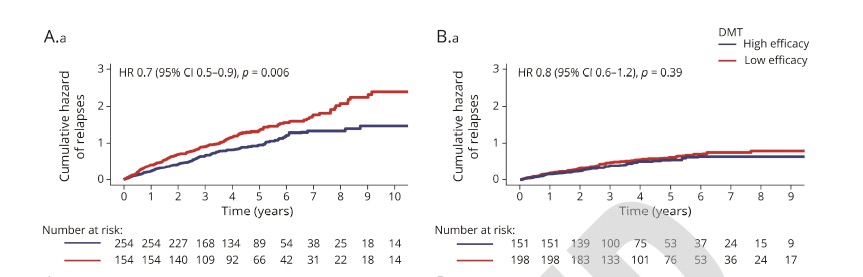
1000名患者被纳入主要分析中。接受高疗效治疗的活动性SPMS患者比接受低疗效治疗的患者复发频率低(危险比[HR]0.7,P=0.006)。
在非活动性SPMS患者中,没有证据表明组间复发频率有差异(HR=0.8,p=0.39)。没有证据表明残疾进展的风险有差异。
这个研究的重要意义在于发现了:在接受治疗的SPMS患者中,高效疗法在减少活动性SPMS患者的复发方面优于低效疗法,但对非活动性SPMS患者来说则不然。然而,更有效的治疗方法在减少该患者群体的残疾进展方面并无优势。
原文出处:
Roos I, Leray E, Casey R, Horakova D, Havrdova E, Izquierdo G, Madueño SE, Patti F, Edan G, Debouverie M, Pelletier J, Ozakbas S, Amato MP, Clavelou P, Grammond P, Boz C, Buzzard K, Skibina O, Ciron J, Gerlach O, Grand'Maison F, Lechner-Scott J, Malpas MPsych CliNeuro C, Butzkueven H, Vukusic S, Kalincik T; MSBase and OFSEP Study Groups. Effects of High and Low Efficacy Therapy in Secondary Progressive Multiple Sclerosis. Neurology. 2021 Jun 30:10.1212/WNL.0000000000012354. doi: 10.1212/WNL.0000000000012354. Epub ahead of print. PMID: 34193589.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#硬化症#
41
#多发性#
40
#Neurol#
45
了解了
62
加强技术指导
65