JCEM:低血浆离子钙与死亡率增加相关
2022-03-18 MedSci原创 MedSci原创
在一般人群中,低血浆离子钙与全因死亡率、癌症死亡率和其他死亡率增加有关,而高水平与心血管死亡率增加相关。
钙是人体内含量最丰富的矿物质,是骨骼的重要结构成分;然而,钙在凝血、细胞内信号传导、肌肉收缩和神经系统功能中也起着重要作用。低钙血症在急诊和重症监护病房中很常见,并且已被发现与患者的疾病严重程度和死亡率相关。然而,血浆钙与普通人群死亡率之间的关系尚不清楚,因为一些研究发现高钙与较高的死亡率相关,而其他研究发现血浆钙与使用总钙或白蛋白调整钙的死亡率之间存在U型关联。低循环总钙或白蛋白调整钙与较高的死亡率相关。
由于生物活性离子钙与死亡率之间的关系尚不清楚。近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,研究人员旨在检验这样的假设,即低血浆离子钙与普通人群全因和特定原因死亡率的较高风险相关。
研究人员纳入了来自哥本哈根一般人群研究的106768名受试者。全因和特定原因死亡率的信息来自登记处,风险是通过STATA命令stcompet使用Cox回归和竞争风险回归计算的。
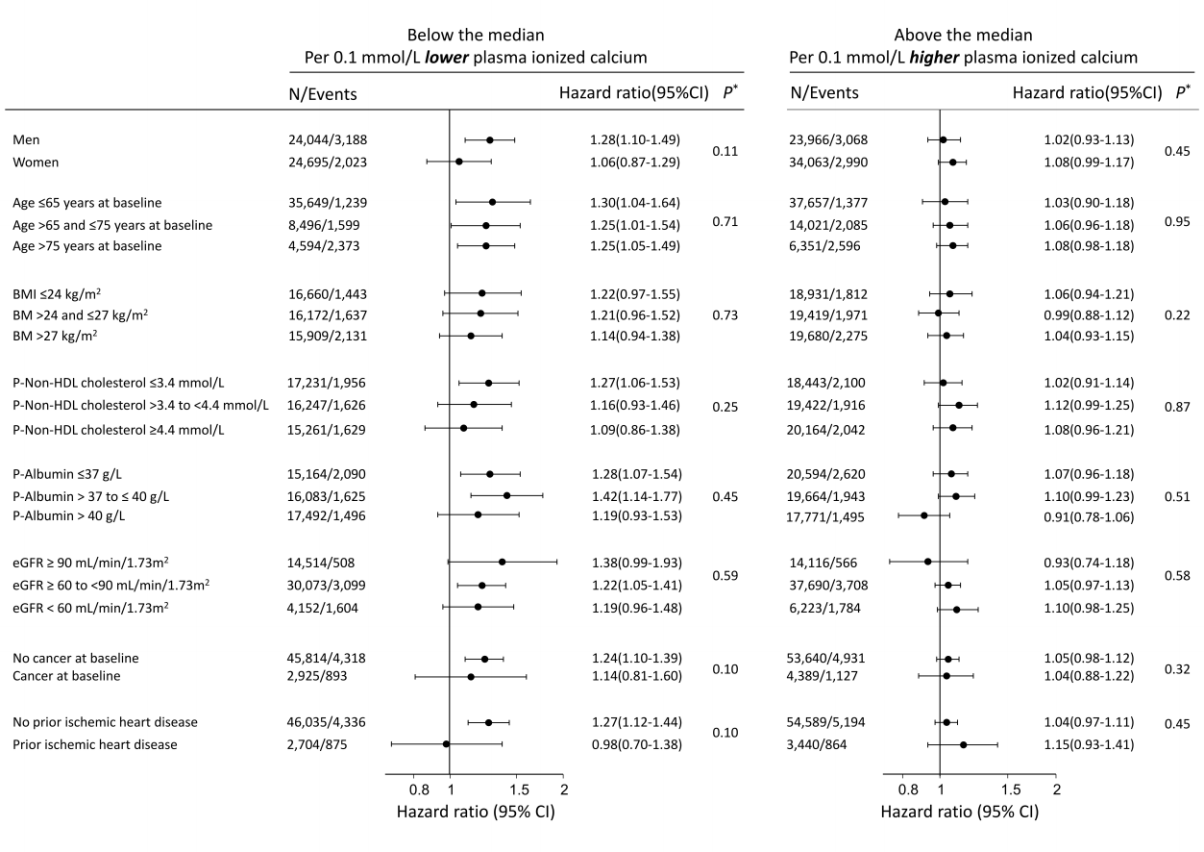
在9.2年的中位随访期间,11269人死亡。血浆离子钙低于中位数1.21mmol/L每降低0.1mmol/L,全因死亡率的多变量调整风险比为1.23(95%CI为1.10-1.38),癌症和其他死亡率的相应风险比分别为1.29(1.06-1.57)和1.24(1.01-1.53)。相比之下,对于心血管死亡率,只有高血浆离子钙与死亡率相关,其血浆离子钙每高于中位数0.1mmol/L的死亡风险比为1.17(1.02-1.35)。研究人员发现血浆离子钙与既往存在的心血管或肾脏疾病对全因死亡率没有相互作用。
在一般人群中,低血浆离子钙与全因死亡率、癌症死亡率和其他死亡率增加有关,而高水平与心血管死亡率增加相关。
原始出处:
Camilla J Kobylecki,et al.Low plasma ionized calcium is associated with increased mortality: a population-based study of 106,768 individuals.JCEM.2022.https://academic.oup.com/jcem/advance-article-abstract/doi/10.1210/clinem/dgac146/6547248?redirectedFrom=fulltext
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#JCE#
31
#JCEM#
29
学习
38